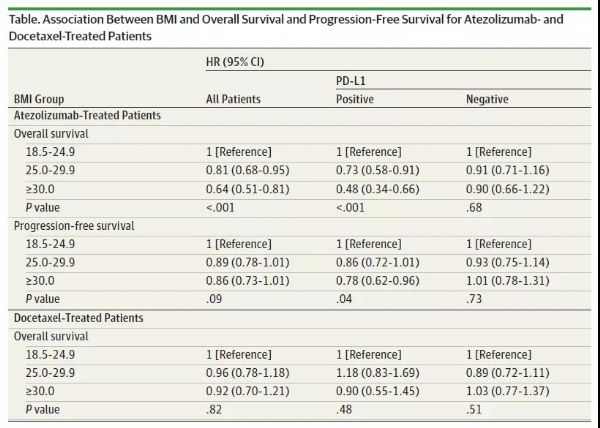
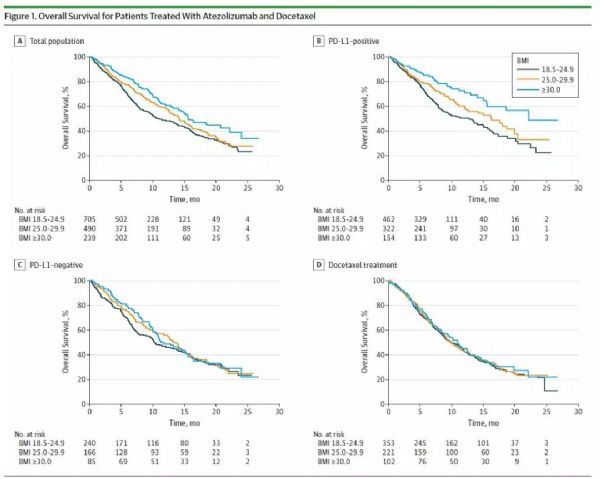
JAMA Oncol:惊人发现!癌症患者越胖,PD-L1抑制剂疗效越好
2020-01-09 不详 BioWorld
导 读:身体质量指数(BMI)是国际上常用的衡量人体肥胖程度和是否健康的重要标准,BMI=体重/身高的平方。BMI较高通常被认为与癌症、糖尿病、心血管疾病以及其它疾病有关。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Oncol#
40
#PD-L1抑制剂#
46
#抑制剂#
36
#PD-L1#
44
#癌症患者#
38
谢谢梅斯提供这么好的信息,学到很多
42
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
44
谢谢梅斯分享这么多精彩信息
51