ESMO Open:西地尼布联合化疗治疗复发性卵巢癌的3期试验结果
2021-02-22 Nebula MedSci原创
西地尼布(Cediranib)是一种口服的抗血管生成的VEGF受体1-3抑制剂
西地尼布(Cediranib)是一种口服的抗血管生成的VEGF受体1-3抑制剂。在一项随机试验中,西地尼布(20 mg/日)与以铂为基础的化疗相结合,作为维持治疗用于首次复发的“铂敏感型”卵巢癌患者,已被证明可以改善患者的无进展生存率(PFS)。
ICON6(NCT00532194)是一项国际性的三臂、双盲、安慰剂对照的随机试验。在2007年12月-2011年12月期间,456名卵巢癌患者被随机分成三组,一组全程接受化疗+安慰剂(A组,对照);一组同时接受化疗+西地尼布,然后安慰剂维持(B组,实验组1);一组同时接受化疗+西地尼布,然后西地尼布维持(C组,实验组2)。主要终点成为A组和C组间的PFS对比,次要终点为总存活率(OS)。
总预后
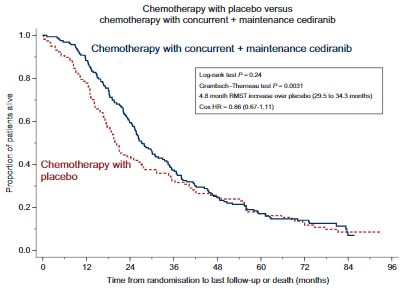
中位随访了25.6月,C组的PFS明显优于A组(危险比[HR] 0.56,95%CI 0.44-0.72,P<0.0001)。在这份最新的生存分析报告中,90%的患者已经死亡。C组和A组的中位生存期相差7.4月(HR 0.86[95%CI 0.67-1.11],P=0.24)。
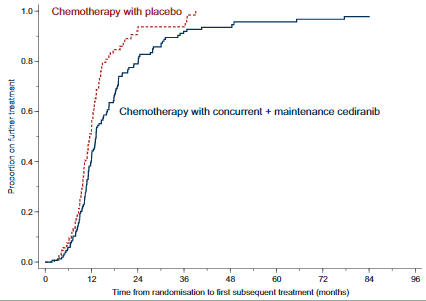
从随机分组到后续治疗的时间
强有力的证据表明,使用Grambsch-Therneau检验偏离了非比例假设(P=0.0031),使得HR难以解释。因此,采用限制性平均生存时间(RMST),6年以上的估计差值为4.8个月(95%CI 0.09-9.74个月)。
尽管无进展生存期在统计学上有显著差异,但死亡风险相对降低14%在传统上没有统计学意义。总体上,在该研究中,PFS的改善和平均生存时间的增加表明,西地尼布在治疗复发性卵巢癌方面可能具有一定活性,应该进一步进行研究。
原始出处:
Ledermann J A,Embleton-Thirsk A C,Perren T J et al. Cediranib in addition to chemotherapy for women with relapsed platinum-sensitive ovarian cancer (ICON6): overall survival results of a phase III randomised trial. ESMO Open, 2021, 6: 100043.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#复发性#
37
#PE#
44
#SMO#
49
#西地尼布#
52
#ESMO#
49
#复发性卵巢癌#
29
#联合化疗#
37
#3期试验#
43