Neurology:CT/MRI灌注成像识别血栓摘除术后大脑无复流,与治疗并发症、3月不良预后相关
2022-01-08 Naomi MedSci原创
近日,有研究人员对3个前瞻性的国际多中心血栓摘除术随机对照试验进行了合并分析。研究证实,脑无复流很常见,可以利用临床上现成的序列通过其特征性的灌注成像曲线来检测,并且与治疗后的并发症和依赖或死亡有关。
在大血管闭塞导致的急性缺血性卒中患者中,尽管有相当大比例的患者及时且成功地进行了血管造影再灌注,但仍有相当一部分患者的功能转归较差。这种未能从明显的治疗成功中获得临床益处的原因尚不清楚,可能与发病前的生理储备不足、介入前的梗死生长以及治疗后的并发症(如再闭塞、出血性转化和脑水肿)有关。更好地理解潜在的机制可能会找到提高治疗效果的新途径。
组织再灌注已被证明是比动脉再通更强的决定临床结果的因素。相反,尽管大血管重建,但不完全微循环再灌注造成的持续性组织少血症(‘无复流’现象)可能会导致较差的恢复。这种现象在冠脉循环中被公认为是不良结果的独立预测因子,在临床实践中经常出现,发生率>50%。与上游动脉闭塞引起的低灌注严重减少下游血液流动相比,这是低灌注的机制。尽管更大的动脉提供了丰富的血液供应,周细胞收缩、内皮细胞肿胀、白细胞和微血栓引起的微血管阻塞可能会损害毛细血管床的灌注。冠状动脉无复流是一种放射学现象,在心外膜动脉再通后,冠脉无复流可立即在术中血管造影中明显表现为远端血流迟缓和心肌潮红减少。目前心脏病学研究中评估和诊断冠状动脉无复流的金标准是在心肌梗死后第1周进行心脏MRI检查。无复流表现为冠脉造影评估的上游大血管状态与下游大血管状态不匹配。微血管组织水平灌注在造影增强MRI上评估,在经皮冠状动脉介入术后再通心外膜动脉的患者中,用钆注射后梗死心脏组织内部的低强化区域是明显的。自1968年首次被描述以来,在临床前研究中,无复流也一直在大脑中被证实。最近的实验数据进一步表明,在最初的24小时内,大脑中存在无复流,并且可能通过药理周细胞松弛和减少中性粒细胞相关的毛细血管停滞而可逆。
尽管有令人信服的临床前证据,大脑无复流的存在仍然存在争议。迄今为止,关于无复流的临床资料有限,部分原因是在早期研究中很难准确地确定血管状态而不采用侵入性诊断性血管造影。最近的4项研究评估了血栓摘除术后的无复流,但报道的发生率从3% 到43% 差别很大。
为了解决人类卒中无复流的不确定性,近日,有研究人员对3个前瞻性的国际多中心血栓摘除术随机对照试验进行了合并分析,这些试验采用预先指定的随访灌注成像和核心实验室判定的血管造影评估,以调查脑无复流在人类中的普遍程度,以及它是否与不良的放射学和临床结果相关。
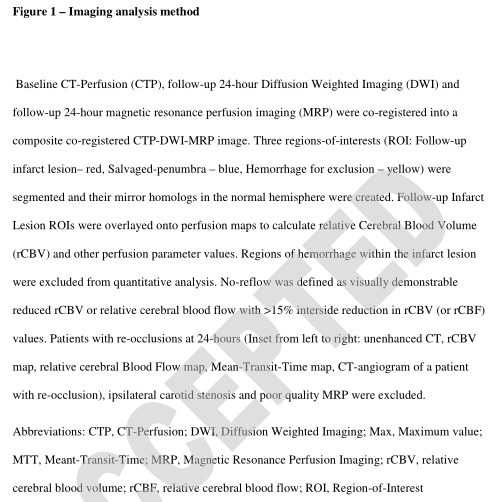
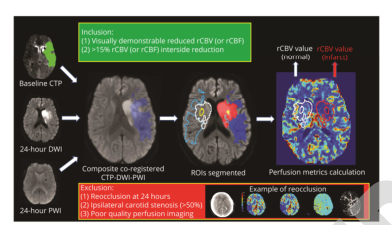
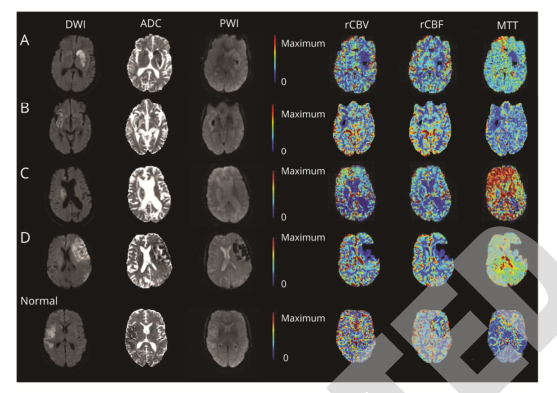
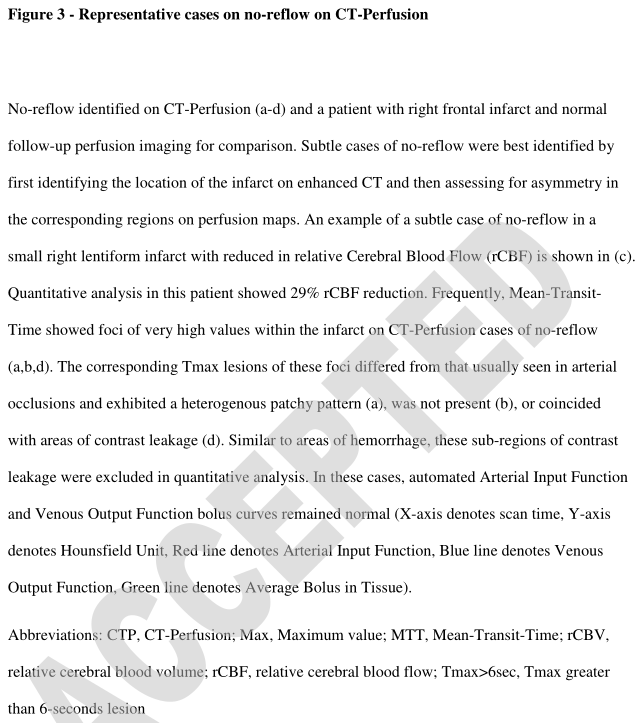
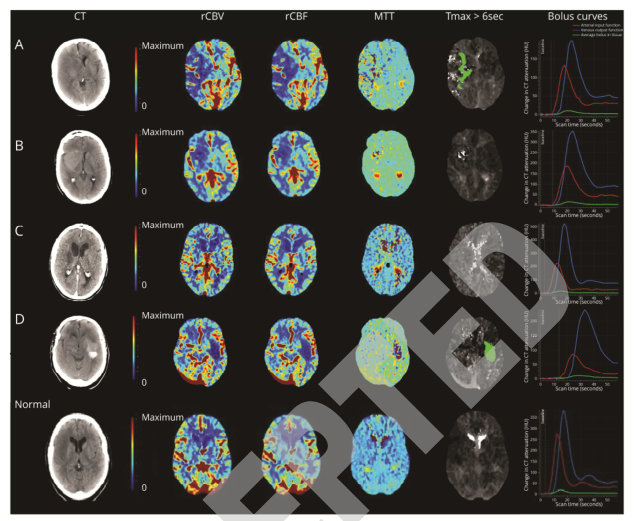
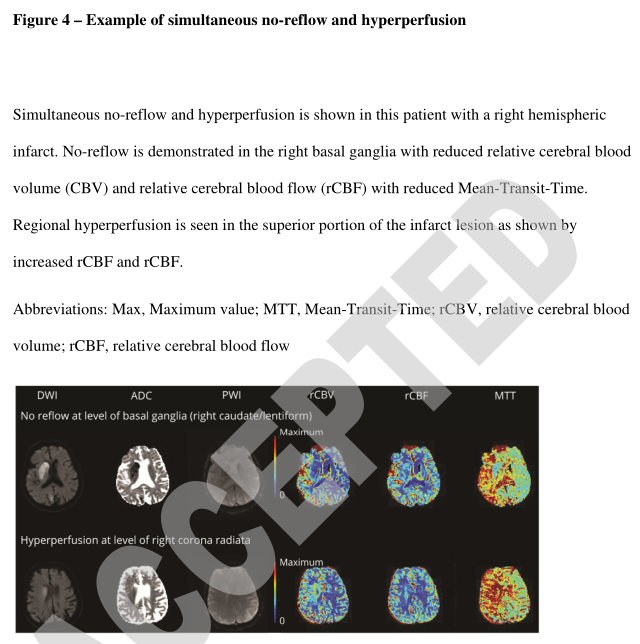
在对EXTEND-IA(ClinicalTrials.gov编号NCT01492725)、EXTENDIA TNK(NCT02388061)和Extended-IA TNK Part-Two(NCT03340493)试验的合并分析中,纳入了接受血栓切除术并接受了脑缺血2c-3评分(前循环大血管闭塞)和24小时随访CT或MRI灌注成像的患者。无复流被定义为在没有颈动脉狭窄或再闭塞的情况下,在相对脑血流量或脑血流图上可见的持续性低灌注区,通过>15%的不对称性进行了定量验证。
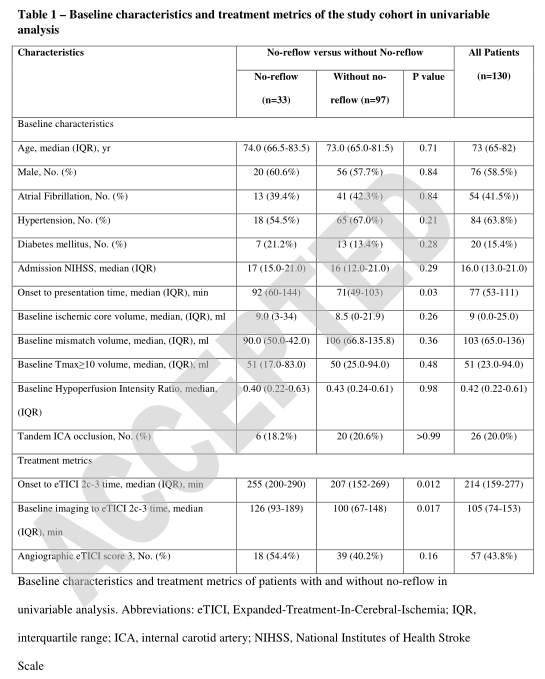
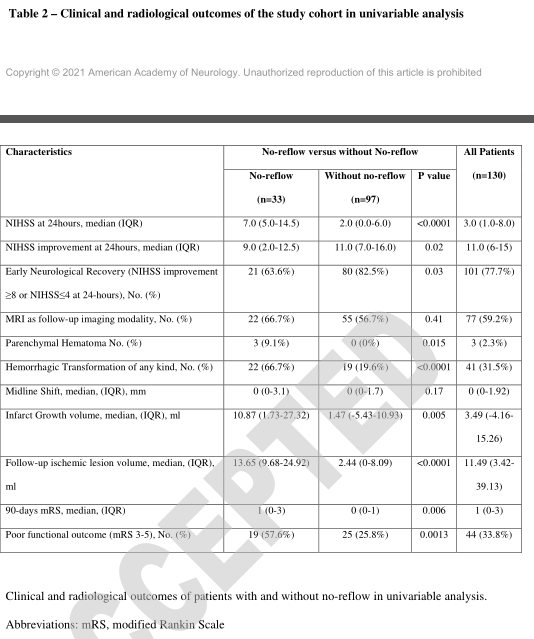
- 130例患者中33例(25.3%)发现无复流区,梗死体积的中位数为60.2%(四分位数范围47.8-70.7%),皮质下(n=26/33,78.8%)和皮质(n=10/33,30.3%)均有无复流区。
- 无复流患者的相对脑血流量中位数为25.2%(四分位数范围16.4%-32.2%,p<0.00001),相对脑血流量为19.1%(四分位数范围3.9%-28.3%,p=0.00011)。梗死区平均通过时间缩短(中位数-3.3%,四分位数范围-11.9-24.4%,p=0.24)。
- 无复流患者和无复流患者的基线特征相似。
- 在多变量分析中,无复流的存在与出血性转化(AOR=1.79,95%CI2.32-15.57,p=0.0002)、更大的梗死增长(β=11.00,95%CI5.2216.78,p=0.00027)、24小时内美国国立卫生研究院卒中评分改善降低(β=-4.06,95%CI-6.78-1.34,p=0.004)以及90天后残疾或死亡有关(AOR=3.72,95%CI为1.35~10.20,p=0.011)。
脑无复流很常见,可以利用临床上现成的序列通过其特征性的灌注成像曲线来检测,并且与治疗后的并发症和依赖或死亡有关。有必要进一步研究血管造影再灌注后无血流在继发性损伤中的作用。
这项研究提供了第二类证据,证明在CT/MRI灌注成像上24小时的脑无复流与治疗后的并发症和不良的3个月功能结果有关。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#Neurol#
29
#CT/MRI#
32
#并发#
37
求原文🙏
54
涨知识了
47
好文章,值得一读。
52
#灌注成像#
36
认真学习了
48
学习学习我学习学习学习学习学习学习学习学习学习学习学习
56
太棒了
28