吸烟竟引发结直肠癌!中国3亿烟民,近一半会因吸烟早逝...
2022-05-31 Swagpp MedSci原创
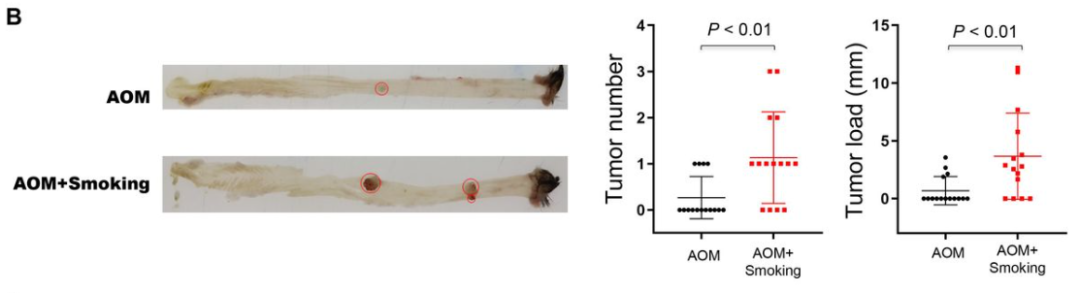
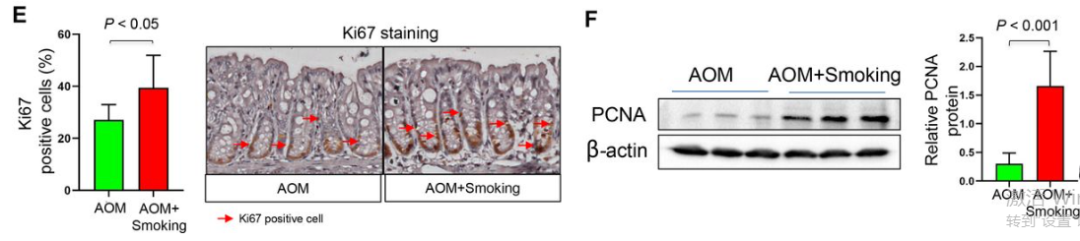
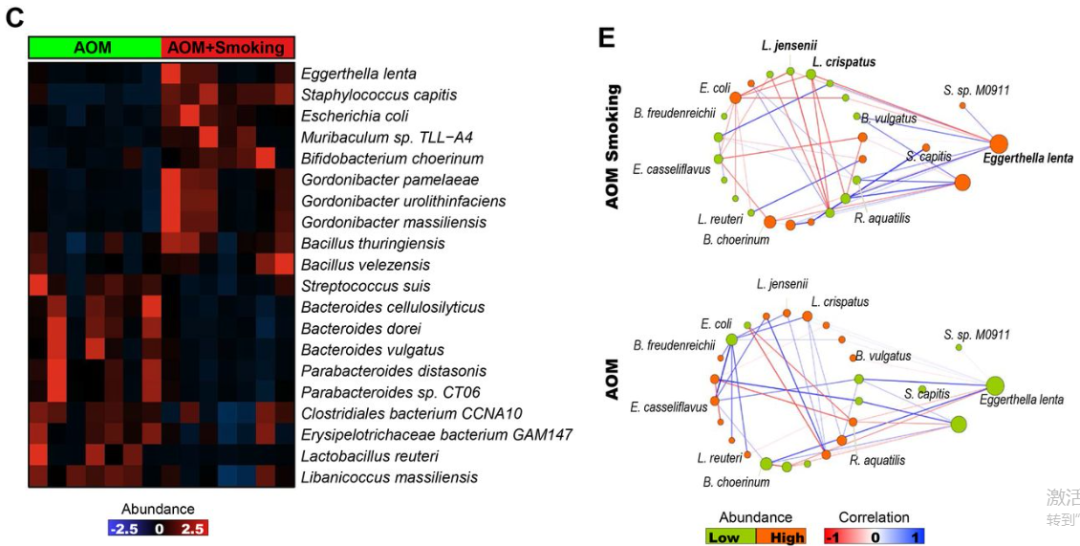
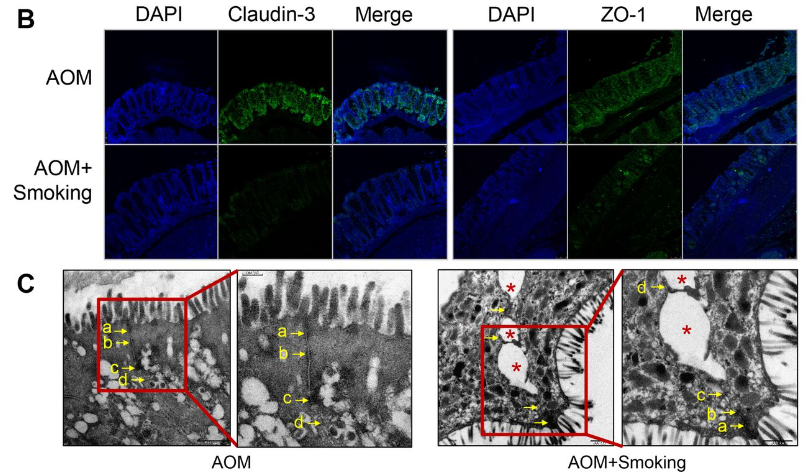
GUT:香烟烟雾会导致肠道菌群失调,进而改变肠道代谢物且损害肠道的屏障功能,可能会激活结肠上皮细胞的致癌MAPK/ERK信号传导,诱发结直肠癌的发生。

王辰院士在2022年世界无烟日主题活动发表演讲
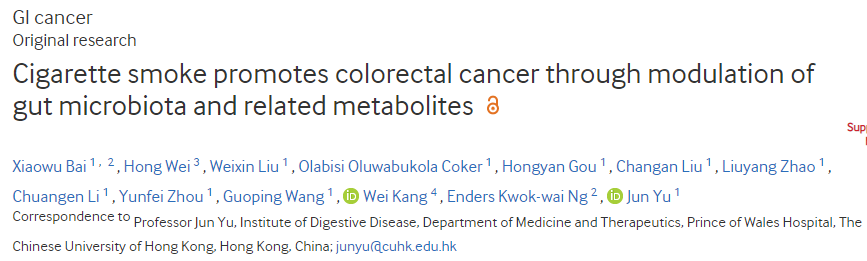 DOI: 10.1136/gutjnl-2021-325021
DOI: 10.1136/gutjnl-2021-325021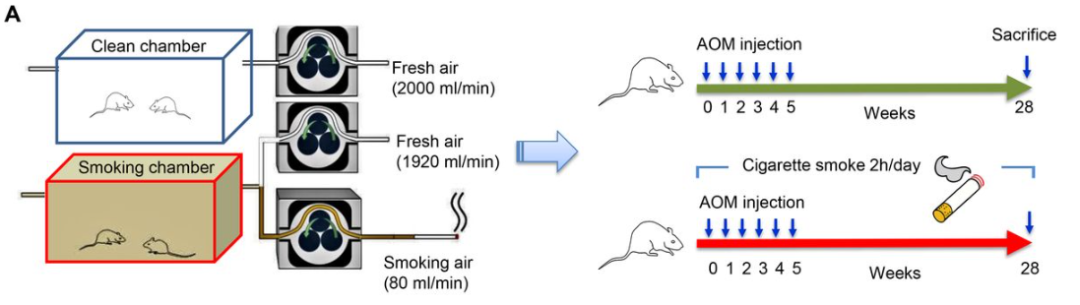
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#结直肠#
33
感谢分享
56
好东西 谢谢分享
61
#学习##期刊论坛#
77
不错的文章
64