PLoS One:乙肝新药2a期临床出色,有望带来功能性治愈
2017-05-25 佚名 药明康德
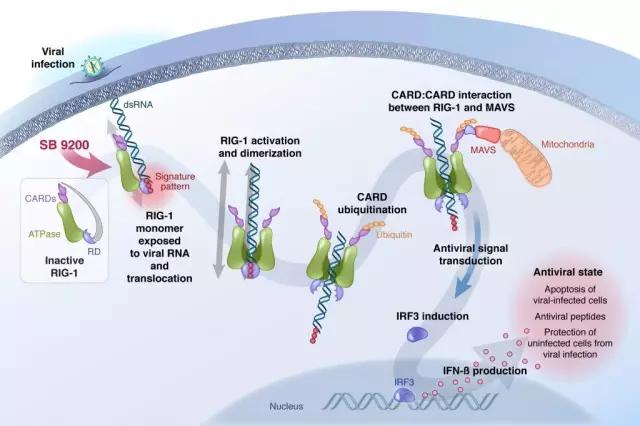
近日,位于马萨诸塞州的Spring Bank Pharmaceuticals宣布,其在研新药SB 9200在治疗慢性乙肝的2a期临床中取得了出色的成果,这也有望将这一新药推进到临床的下一个阶段。乙肝是一种影响广泛的肝脏疾病。据世界卫生组织估计,全世界范围有2.4亿人慢性感染乙型肝炎,每年有超过78万人死于乙型肝炎并发症,包括肝硬化和肝癌。中国是一个乙肝感染大国,全国至少有1亿慢性乙型肝炎病毒(HB
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Plos one#
34
#乙肝新药#
22
#功能性#
0
期望啊。
48
不错,拭目以待!
44