NEUROLOGY:无效再通治疗的多变量预测模型有助于急性缺血性卒中患者临床决策
2022-09-10 影像小生 MedSci原创
预测算法将有助于为共享决策提供信息,并设定现实的期望。尽管该算法在医疗资源高的情况下拒绝治疗的临床效益和可用性有待于未来的研究,但开发一种预测FRT的可靠算法似乎是可以实现的,并应纳入更先进的入院影像
尽管机械取栓术(MT)治疗大血管急性缺血性卒中(AIS)的疗效显著,但在随机对照试验中1 / 5的患者和在现实环境中1 / 3的患者有很差的长期预后(改良Rankin量表[mRS], 90天5 - 6),尽管技术上是成功的干预。“无效干预”一词就是为了解释这一问题而创造的。同样,接受静脉溶栓(IVT)的患者中有1 / 5的患者长期预后很差,尽管有最好的可用治疗,老年患者的患病率甚至更高。
尽管大约 1/4缺血性卒中患者IV 溶栓 (IVT) 和机械血栓切除术 (MT) 的结果非常差,并且与高经济负担相关。伯尼尔大学医院Thomas Raphael Meinel等为开发和验证一个多变量预后模型,以识别接受这些治疗的患者中的无效的血管再通治疗 (FRT)。
前瞻性收集接受 MT 和/或 IVT 治疗的患者。数据集分为训练 (N = 1,808, 80%) 和内部验证 (N = 453, 20%) 队列。在对入院时可用的 32 个变量进行 K最近邻填充后,使用梯度增强决策树机器学习模型来预测FRT(定义为 3 个月时改进Rankin 量表 5-6 分)。并报告特征重要性、辨别能力、校准和决策曲线分析。
共纳入2,261 名患者,中位(四分位距)年龄为 75 岁(64-83 岁),46% 为女性,中位 NIH 卒中量表评分为 9(4-17),34%患者只接受了IVT,41%患者只接受了MT,以及 25%接受桥接治疗。
最终,539人 (24%)为 FRT,与单独 IVT (11%) 相比,更多见于单独 MT (34%)。
特征重要性将临床变量(卒中严重程度、年龄、活动性癌症、卒中前残疾)、实验室值(葡萄糖、C 反应蛋白、肌酐)、成像生物标志物(白质高信号)和发病至入院时间确定为最重要的预测因子。
mRS 5-6预测模型的性能
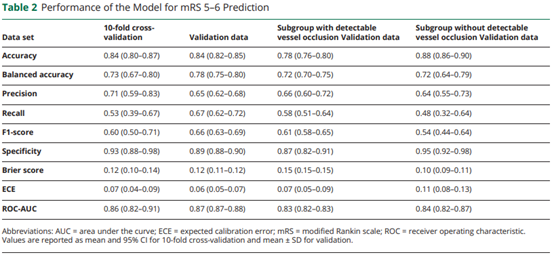
最终模型在预测 3 个月 FRT(曲线下面积 0.87, 95% CI 0.87–0.88)方面具有区分性,并且具有良好的校准(Brier 0.12, 0.11–0.12)。整体表现中等(F1-score 0.63 ± 0.004),决策曲线分析表明,治疗阈值越低(高达0.8),平均净效益越高。
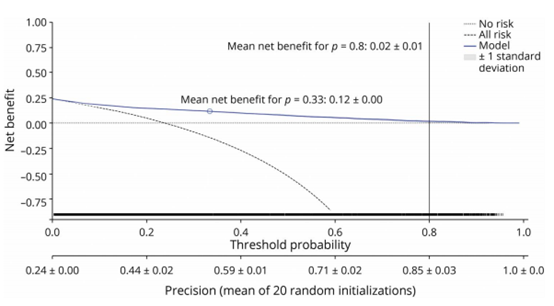
xgb分类器决策曲线分析
这种 FRT 预测模型可以帮助为共同决策提供信息,并确定紧急情况下最相关的特征。尽管它在资源匮乏的医疗保健环境中可能特别有用,但有必要结合更多的多方面变量以进一步提高预测性能。
原文出处
Multivariable Prediction Model for Futile Recanalization Therapies in Patients With Acute Ischemic Stroke. Neurology Sep 2022, 99 (10) e1009-e1018; DOI: 10.1212/WNL.0000000000200815
https://doi.org/10.1212/WNL.0000000000200815
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#缺血性卒#
40
#缺血性#
46
#临床决策#
45
#Neurol#
41
#卒中患者#
40
#缺血性卒中患者#
37
#预测模型#
0
#决策#
45