Nat Commun:在培养皿中模拟声带对香烟烟雾的反应
2019-09-29 Nature自然科研 Nature自然科研
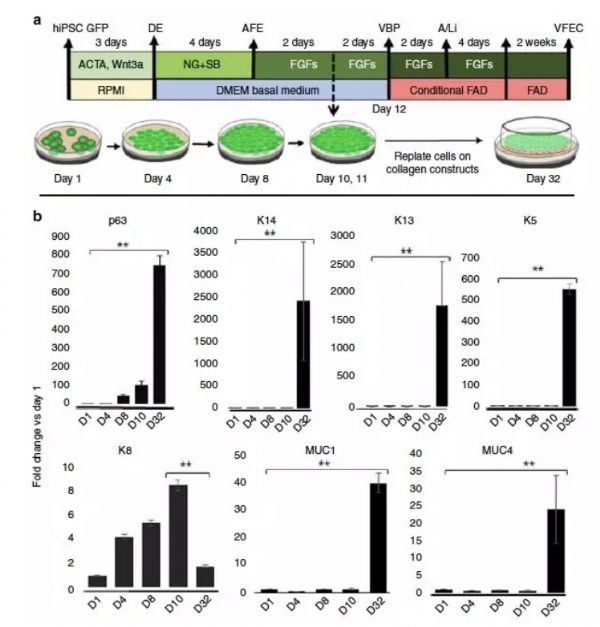
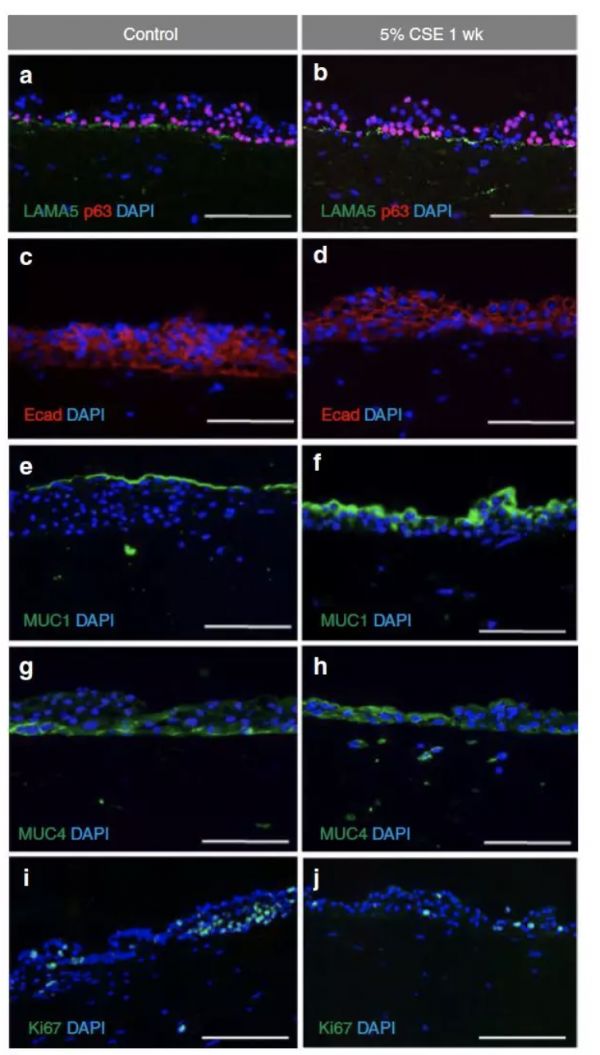
《自然-通讯》本周发表的一项研究Human induced pluripotent stem cell-derived vocal fold mucosa mimics development and responses to smoke exposure报道了人声带组织(即粘膜)的一个实验室三维模型。当暴露在香烟烟雾中时,该组织会出现在人喉中发现的反应,即炎症。该模型可用于对声带疾病或损害的相关
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Nat#
21
#COMMUN#
15
#香烟#
24
学习了
52
好好好好好好
43