Circulation:随机临床试验结果表明难治性房颤微创外科消融疗效好于导管消融
2012-07-27 倚天观海 丁香园
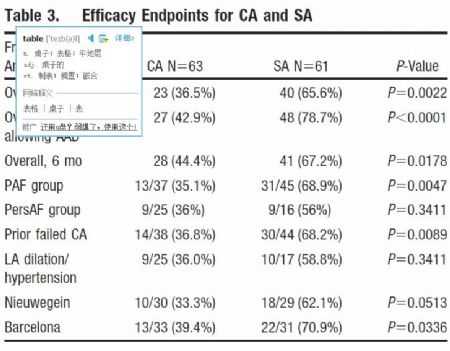
图:导管消融和微创外科消融的有效性终点 导管消融(CA)和微创外科消融(SA)已成为抗心律失常药物难治性心房颤动的可接受治疗。随着两项技术的日渐成熟,关于CA和SA地位的争议就一直不断,此前尚无头对头比较两者疗效和安全性试验存在。这项名为的FAST研究是首个随访12个月比较他们的疗效和安全性的随机临床试验。 124例抗心律失常药物难治性心房颤动患者被纳入本研究。其中42名患者(43%)伴有左房
图:导管消融和微创外科消融的有效性终点
导管消融(CA)和微创外科消融(SA)已成为抗心律失常药物难治性心房颤动的可接受治疗。随着两项技术的日渐成熟,关于CA和SA地位的争议就一直不断,此前尚无头对头比较两者疗效和安全性试验存在。这项名为的FAST研究是首个随访12个月比较他们的疗效和安全性的随机临床试验。
124例抗心律失常药物难治性心房颤动患者被纳入本研究。其中42名患者(43%)伴有左房扩大和高血压,82名患者(67%)此前行导管消融失败。这些患者随机分配至导管消融组(63名)和微创外科消融组(61)。导管消融包括线性窦肺静脉隔离和可选的附加线消融。外科微创消融包扩双边肺静脉、心脏神经丛双极射频隔离,可选的附加线切除左心耳。在6至 12 个月的随访中进行心电图和 7 天动态心电图记录。
研究结果显示SA组较CA组更为有效:疗效性研究的主要终点为12月后不服用抗心律失常药物无持续30秒以上的左房性心动过速。在CA组为36.5%,SA组为65.6%(p值0.0022)。两组间的亚组分析未显示差异。12月随访期内严重不良事件的主要安全终点,在SA组明显高于CA组,分别为21例(34.4%)和10例(15.9%),p值0.027。严重不良事件主要包括气胸、大出血、需安装起搏器等。在导管消融组,有1名患者在一个月内因蛛网膜下腔出血死亡。
研究者由此得出结论,在对伴左房扩大和高血压或以经过导管消融治疗失败的难治性心房颤动患者,微创外科消融治疗疗效较好,能获得更多的12月后无左房性心动过速发作的结果。但在严重不良事件发生率方面微创外科消融明显要高于导管外科消融。
这一研究将在临床医生进行治疗决策时提供更多的信息。
原文链接:
Boersma LV, Castella M, van Boven W, Berruezo A, Yilmaz A, Nadal M, Sandoval E, Calvo N, Brugada J, Kelder J, Wijffels M, Mont L. Atrial fibrillation catheter ablation versus surgical ablation treatment (FAST): a 2-center randomized clinical trial. Circulation. 2012 Jan 3;125(1):23-30.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#随机临床试验#
29
#微创#
32
#导管消融#
34
#消融#
40
#难治性#
37
#微创外科#
29