ACR 2015:老年人发生骨折,死亡风险将翻倍!
2015-11-08 seven L 译 MedSci原创
先前有研究表明老年人髋部骨折会导致骨折后1-2年内死亡风险的增加。近期一项纳入了 238,673名老年人的研究表明,老年人发生骨折会导致过早死亡风险增加。纳入研究时参与者平均年龄63岁,平均随访5.7年后参与者结局如下图:男性死亡率是15.7/1000人年,对于经历了骨折的男性,死亡率上升到33.0/1000人年,增长了约1倍。女性死亡率是7.9/1000人年,经历骨折的老年女性死亡率同样增长1倍
先前有研究表明老年人髋部骨折会导致骨折后1-2年内死亡风险的增加。近期一项纳入了 238,673名老年人的研究表明,老年人发生骨折会导致过早死亡风险增加。
纳入研究时参与者平均年龄63岁,平均随访5.7年后参与者结局如下图:
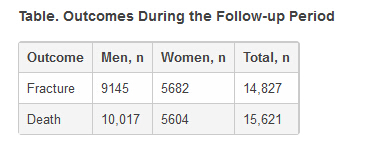
男性死亡率是15.7/1000人年,对于经历了骨折的男性,死亡率上升到33.0/1000人年,增长了约1倍。
女性死亡率是7.9/1000人年,经历骨折的老年女性死亡率同样增长1倍左右,达到了19.0/1000人年。
研究者惊奇地发现,老年人发生的几乎所有的骨折,除了手指和脚趾,均会增加死亡风险。骨质疏松的严重性被低估了。
我们应该告诉老年人骨折会导致其死亡风险增加,事实上,≥70岁的人群在下一年死亡风险为20%-25%,这是一个比诊断癌症还恐怖的数据。当人们了解到骨折会增加寿命减短的的风险,就不会再那么讨厌使用拐杖了。
原始出处:
American College of Rheumatology (ACR) 2015 Annual Meeting: Abstract 3173. Presented November 8, 2015.
Medscape:Fractures Double Risk for Death in Older Adults
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













了解一下!进展!
78
学习了,(◎_◎;)
60
值得关注
169
这篇文章有一定深度
108
是一篇不错的文章
110
不错,赞一个
71
给力
137
真的
81
#死亡风险#
26
#ACR#
26