CARDIOVASC DIABETOL:首发研究!5米步态速度测试可评估老年患者认知和身体状态
2022-02-02 MedSci原创 MedSci原创
建议在体弱的高血压糖尿病老年人的综合老年评估中增加对认知和身体状况的评估。
糖尿病和高血压在老年人中很常见,并且已被确定是导致老年人“虚弱”的危险因素。虚弱是一种多维状态,表示老年人的健康储备降低和对压力源的易感性增加,相关死亡、住院、功能和认知障碍的风险都很高。此外,患有糖尿病和高血压的虚弱患者认知和身体障碍的风险增加。本研究旨在评估患有糖尿病和高血压的体弱老年人的身体和认知障碍之间的相关性。
研究组评估了2021年3月至2021年10月在意大利阿韦利诺(意大利卫生部地方卫生单位)就诊的糖尿病和高血压虚弱老年患者进行了连续评估。纳入标准:既往诊断为糖尿病和高血压,无继发性病因,年龄>65岁,虚弱状态,蒙特利尔认知评估(MoCA)得分<26。
一共有179名患者成功完成了研究。结果发现MoCA评分与5米步态速度测试之间存在强烈且显著的相关性。为了进一步验证这一结果,对潜在的混杂因素进行了线性多变量分析,以MoCA评分作为因变量,同样的这证实了与血糖的显著相关性。

MoCA评分与步态速度测试的离散度模型(气泡图)
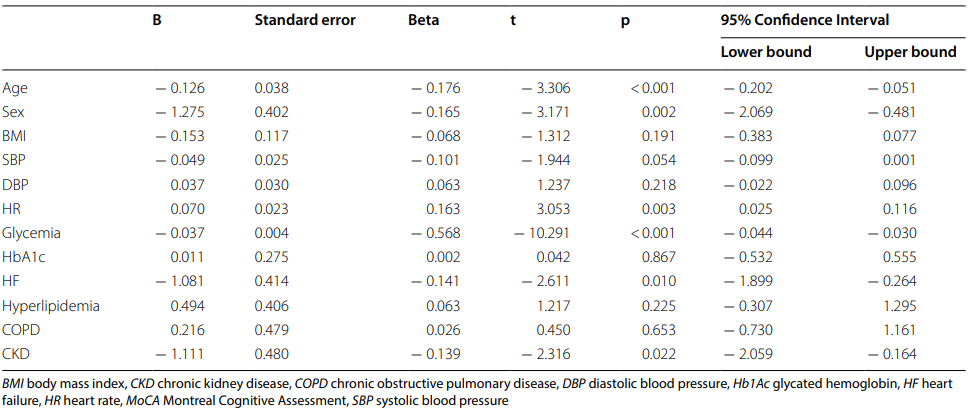
以MoCA评分为因变量的多元回归分析
总之,研究数据表明,使用MoCA和步态速度测试可能有助于评估老年患者认知和身体状态。建议在体弱的高血压糖尿病老年人的综合老年评估中增加对认知和身体状况的评估。这项研究是第一个将体弱的糖尿病和高血压老年人的MoCA评分和5米步态速度测试相关联的研究。有必要对更大的队列进行进一步的分析和后续评估,以证实此结果的准确性。
参考文献:Mone, P., Gambardella, J., Lombardi, A. et al. Correlation of physical and cognitive impairment in diabetic and hypertensive frail older adults. Cardiovasc Diabetol 21, 10 (2022). https://doi.org/10.1186/s12933-021-01442-z
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#ASC#
52
#步态#
46
#DIA#
42
#BET#
59