颠覆常识!气管插管并不能完全阻止反流误吸
2019-01-24 一叶飘零 医学之声
吸入性肺炎是气管插管和长期机械通气的并发症,我们一直认为气管导管的套囊能够封闭气道,保护气道不受分泌物侵袭,但是,套囊确实如我们期许的那样吗?
吸入性肺炎是气管插管和长期机械通气的并发症,我们一直认为气管导管的套囊能够封闭气道,保护气道不受分泌物侵袭,但是,套囊确实如我们期许的那样吗?
我们为什么重视机械通气患者发生反流误吸?
患者发生反流误吸,便有可能导致吸入性肺炎,而吸入性肺炎正是患者围术期死亡的重要原因之一。
吸入性肺炎是指吸入酸性物质、食物、胃内容物或碳氢化合物或其他刺激性液体后,引起的肺损伤。严重者可导致低氧血症或急性呼吸衰竭。
1、术前禁食水的目的便是防止反流误吸
全麻术前禁食水的目的在于减少胃内容物容量,避免出现围手术期胃内容物返流而导致的误吸,原因在于,全麻后,患者正常的保护性气道反射被麻醉药物所抑制,胃内的食物或胃液容易反流误吸,引起患者呼吸道梗阻和吸入性肺炎,甚至窒息死亡。
2、ICU机械通气患者,频繁吸引气管导管也是为了防止反流误吸
在ICU中,机械通气的患者,往往需要频繁吸痰,目的在于将呼吸道分泌物或误吸的呕吐物吸出,以保持呼吸道通畅,预防吸入性肺炎、呼吸困难、发绀,甚至窒息。
3、反流误吸,误吸胃酸最危险
反流误吸的物质有很多,但是最危险的还是胃酸误入气道,死亡率非常高,误吸胃酸的患者,又称为Mendelson综合征
Mendelson综合征是指少量的酸性物质吸入肺内引起的严重肺损伤,常发生在禁食后全麻且意识不清时或意识障碍的患者。
1946年,首先由Mendelson描述,发生于误吸后2~4小时,出现“哮喘样综合症”,24小时X线上可见不规则边缘模糊的斑状阴影的综合症。
患者通常会发生急性的吸入性肺水肿,呈现急性哮喘样发作,明显发绀,甚至造成死亡。
4、为了防止反流误吸,气管导管套囊在不断改进
带套囊的气管导管是为了减少反流误吸的重要措施之一,由于套囊压迫气道,可能造成气道粘膜坏死,气道狭窄的严重并发症,因此目前已经由高压高容发展到低压高容的套囊技术,已期达到更好的密封性,更低的套囊压力。
理论上,如果套囊压力适合,套囊下的气道是不受反流误吸侵袭的。
尽管我们为了减少围手术期吸入性肺炎的发生率和严重程度做出了大量的努力,如术前禁食、术前评估围手术期肺部误吸的危险因素、排空ACh、快速序贯麻醉和环状吸入术,以及使用带套囊的气管导管等措施成功地降低了吸入性肺炎的发生率。
然而,最近的大规模研究发现,围手术期吸入性肺炎任然是导致麻醉相关死亡或不可逆脑损伤的主要原因。
我们传统的观念认为,带套囊的气管导管能够封闭气道,有效防止反流误吸的发生,但是事实真是这样吗?套囊能不能如我们期许的那样完成任务呢?
最新前沿研究表明,气管导管套囊并不能完全阻止反流误吸
目前研究表明,吸入性肺炎是与全麻相关的一个不可忽视的死亡原因,原因可能于全麻下胃液反流有关。例如,气管导管周围潜在的胃液反流可能导致吸入性肺炎。
因此,作者大胆的假设患者拔除气管导管的pH值可能是酸性的,这可能是未诊断出的胃反流的前兆。
为了验证这一假设,作者进行了一项前瞻性的观察性研究,以评估全身麻醉后拔除气管导管的pH值。
设计简单又巧妙,关键在于对于问题的思考,总共对200例接受全身麻醉的患者,拔出的气管导管进行了PH测量。排除标准是全胃、胃食管反流和预期的困难气道患者。
作者将气管导管划分了四个位置,分为1234,理论上1这个位置不应该检测出酸性位置,因为这段在套囊的保护之下,这个点下面不远处便是隆突,属于无菌区域,理论上不会有酸性物质侵袭。
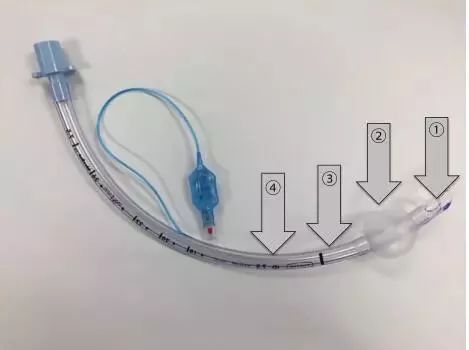
但是结果和我们想的完全相反,尽管这200例患者都没有明显的吸入性肺炎的症状,但是我们却在1和2这个位置检测出了酸性物质。
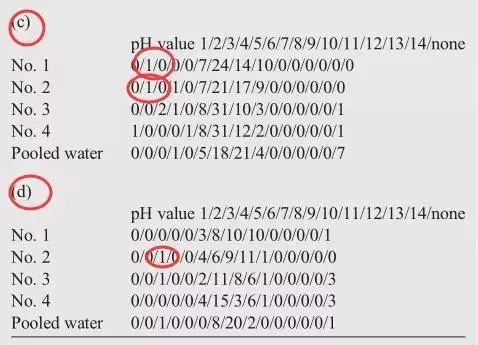
作者研究了四种体位下,气管导管的PH值,a(仰卧位)b(侧卧位)c(头低位)d(俯卧位)
在前两个体位下,未检出酸性物质,在头低位检测出4例,俯卧位1例酸性物质。
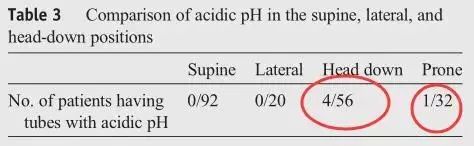
具体到C(头低位)中1、2位置均检测出PH=2的酸性物质,毫无疑问这是胃酸
d(俯卧位)2位置中检测出PH=3的酸性物质
这也就是说,我们平时认为的完全受保护的套囊下位置,也有可能有反流的胃液通过套囊的空隙进入到肺部,如果患者是一个高危患者,肺部本身调节能力较差或者一般状况较差的患者,那么就会造成严重的肺炎,而术后肺炎这个并发症,便足以夺走患者的性命。
有作者不免会有疑问,这个发生的几率并不高,后果也不严重,而忽略了作者选择患者的前提是没有胃食管反流的患者,如果患者换成胃食管反流的患者,无疑,发生的几率以及严重程度,都会较普通患者严重许多。
虽然,这是个前瞻性的研究,但是,我们不得不改变一个观念,即使是充满气体的套囊并不能完全保护患者的气道不受反流误吸的侵袭,因此如果是具有高危的胃食管反流的患者,或是特殊体位的患者,我们仍然要谨慎的防止吸入性肺炎,要反复的吸引口鼻部的分泌物,防止酸性的胃液进入气道,引起严重的反流性肺炎。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











求文献出处
13
请求文献的出处?
49
求文献的出处!
85
文献出处未注明
68
#反流误吸#
41
学习学习再学习再
67
#气管插管#
36
#反流#
27
好
62
学习气管插管的新知识
56