胸椎椎管内硬膜外海绵状血管瘤1例
2019-05-22 华德河 郝其全 孙海燕 脊柱外科杂志
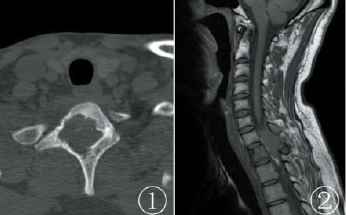
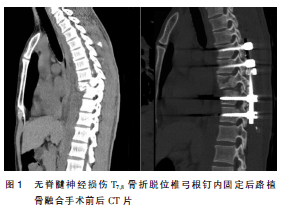
患者男,48岁,因“渐进性双下肢麻木、无力1年,加重6个月”于2017年10月14日收住院。10年前因高处坠落伤致T4椎体压缩性骨折(图1a,b),伤后即感胸背部持续性钝痛,躯干及四肢感觉运动正常,经卧床休息等非手术治疗3个月后恢复正常生活。近1年出现感觉减退,由双下肢远心端向近心端渐进性发展,近10d发现双下肢渐进性无力,可站立、行走。查体示双侧肋弓以下平面痛、温觉及触觉减退,双下肢肌力4级,肛
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#椎管内#
35
#硬膜外#
38
#椎管#
29
#血管瘤#
35
#胸椎#
30
#海绵状血管瘤#
31
#海绵状#
35