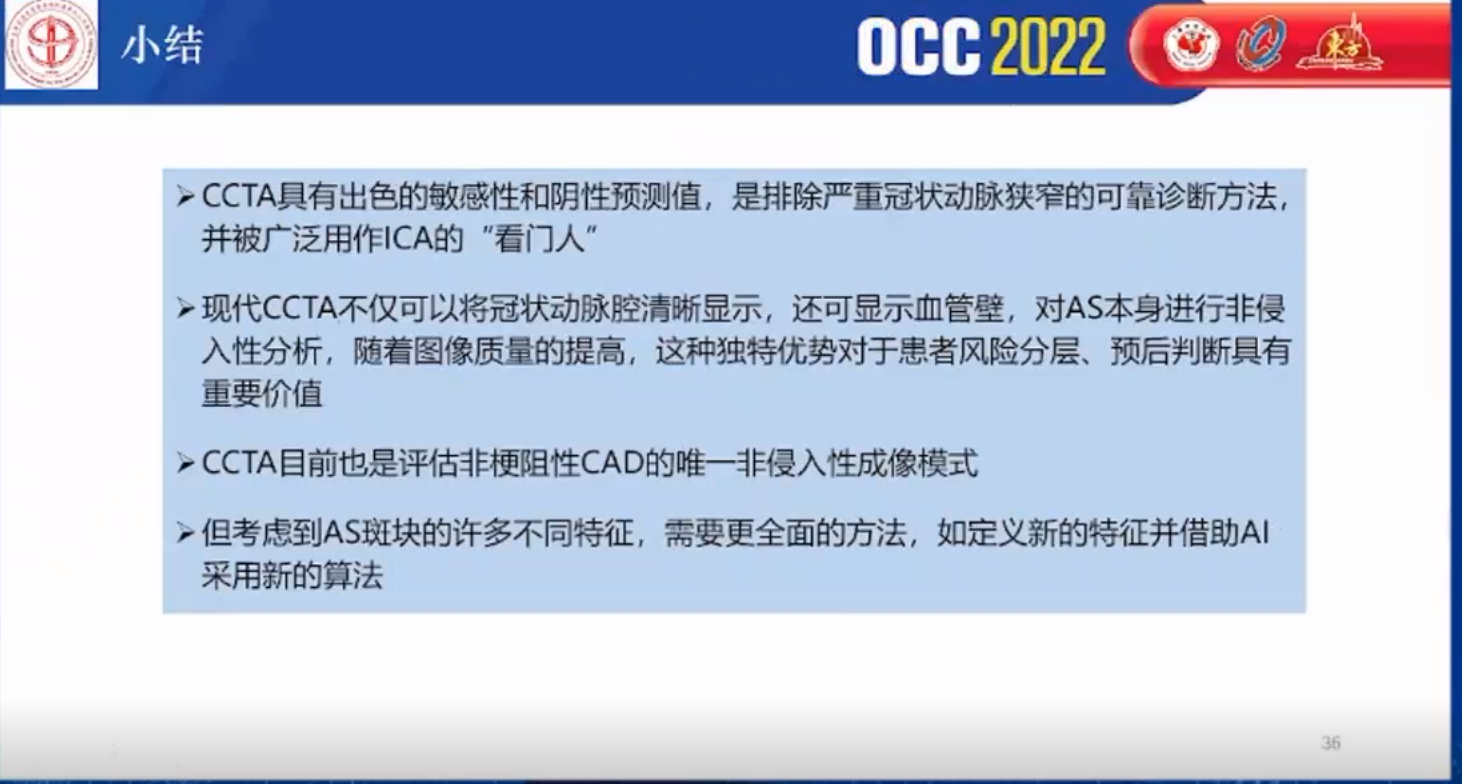
OCC 2022:张俊峰教授冠脉CT斑块的判断和评估
2022-05-26 MedSci原创 MedSci原创
OCC大会播报。张俊峰教授:冠脉CT斑块的判断和评估。
ACC根据动脉粥样硬化病变过程将其细分为6型。
Ⅰ型脂质点。动脉内膜出现小黄点,为小范围的巨噬细胞含脂滴形成泡沫细胞积聚。
Ⅱ型脂质条纹。动脉内膜见黄色条纹,为巨噬细胞成层并含脂滴,内膜有平滑肌细胞也含脂滴,有T淋巴细胞浸润。
Ⅲ型板块前期。细胞外出现较多脂滴,在内膜和中膜平滑肌层之间形成脂核,但尚未形成脂质池。
Ⅳ型粥样斑块。脂质积聚多,形成脂质池,内膜结构破坏,动脉壁变形。
Ⅴ型纤维粥样斑块。为动脉斑块粥样硬化最具特征性的病变,呈白色斑块突入动脉腔内引起管腔狭窄。斑块表面内膜被破坏而由增生的纤维膜(纤维帽)覆盖于脂质池之上,病变并可向中膜扩展,破坏管壁,并同时可有纤维结缔组织增生,变性坏死等继发病变。
Ⅵ型复合病变。为严重病变,由纤维斑块发生出血、坏死、溃疡、钙化和附壁血栓形成。粥样斑块科因内膜表面溃破而形成所谓粥样溃疡。破溃后粥样物质进入血流成为栓子。

易损斑块的的类型,来源:Circulation. 2003 Oct 7;108(14):1664-72.
目前临床上有很多侵入性的检查,例如OCT、IVUS等。但是有创的手段往往发生在患者已经有明显的临床症状或者临床事件之后,往往不能够达到早发现、早处置的目的。ct作为一种无创的的检查手段如果可以将症状不典型的或者不愿意做有创检查的患者及早发现易损斑块,才是我们降低猝死风险的有效手段。
易损斑块特征:低衰减斑块
- 斑块的成分可通过CT值体现,钙化成分CT值最高,其次是纤维成分,脂质成分CT值最低
- 低衰减斑块是指CT值最低、最容易破裂的脂质斑块,一般研究中定义为<30HU
- 但斑块CT值受到造影剂、斑块体积、层厚、球管电压等多种因素影响,再加上脂质斑块与纤维斑块的CT值存在重叠,单纯使用CT值区分存在困难
- 因此目前的研究中主要依靠特殊程序来识别哪些斑块是低衰减斑块。
需注意,低衰减斑块与严重的巨噬细胞浸润和大的脂质坏死核心密切相关,<60HU的斑块像素相关区域也可准确检查出富含脂质的斑块。
易损斑块特征:“餐巾环”征
指在低密度斑块周围围绕着一圈高密度环,环的密度大于内核但但不到钙化,产生“餐巾环”征的原因是斑块的坏死核比较大,可以在CT的横截面上显示出来,环是斑块中的纤维成分。
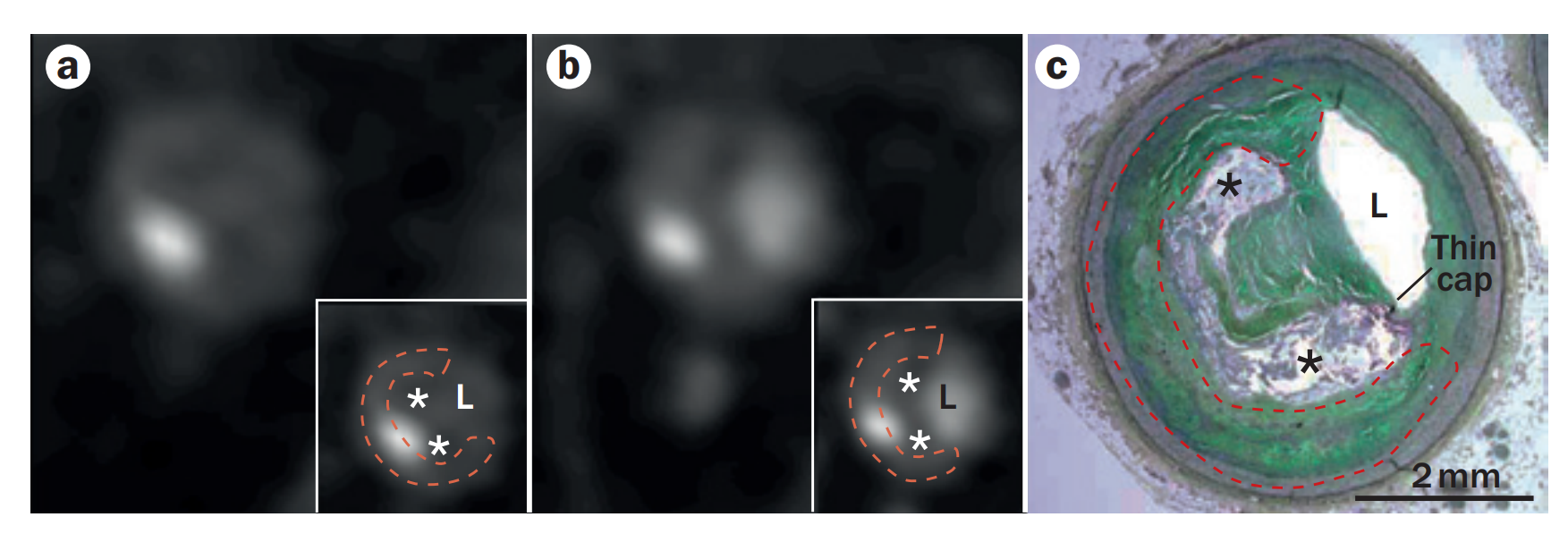
a:未增强扫描横断面CT b:增强扫描横断面CT

易损斑块特征:正性重构
- 指在有冠脉粥样硬化的血管壁,当斑块持续增大,血管壁也会发生代偿性的增大,从而维持管腔内的有效面积。
- 正性重构与丰富的巨噬细胞和激增的坏死中心有关。
- 重构指数∶病变段的最大血管直径(包括斑块和管腔)与斑块两端的平均直径之间的比值。重构指数≥1.1为正性重构。
相对于蒂塔的高危斑块CT特征(如低衰减和点状钙化),正性重构对鉴别易损斑块的价值更高。
易损斑块特征:点状钙化
指冠状动脉管壁内局灶性钙化病变在任意方向测得最大直径<3mm,且平均密度>130HU的高密度灶。但是目前相关研究结果差异较大,难以确定点状钙化与斑块破裂有关。普遍认为微笑钙化科作为不稳定型冠心病的常用检测指标。

除了上述易损斑块的研究特征。最新还发现了一个生物标志物可以也可以提示易损斑块。
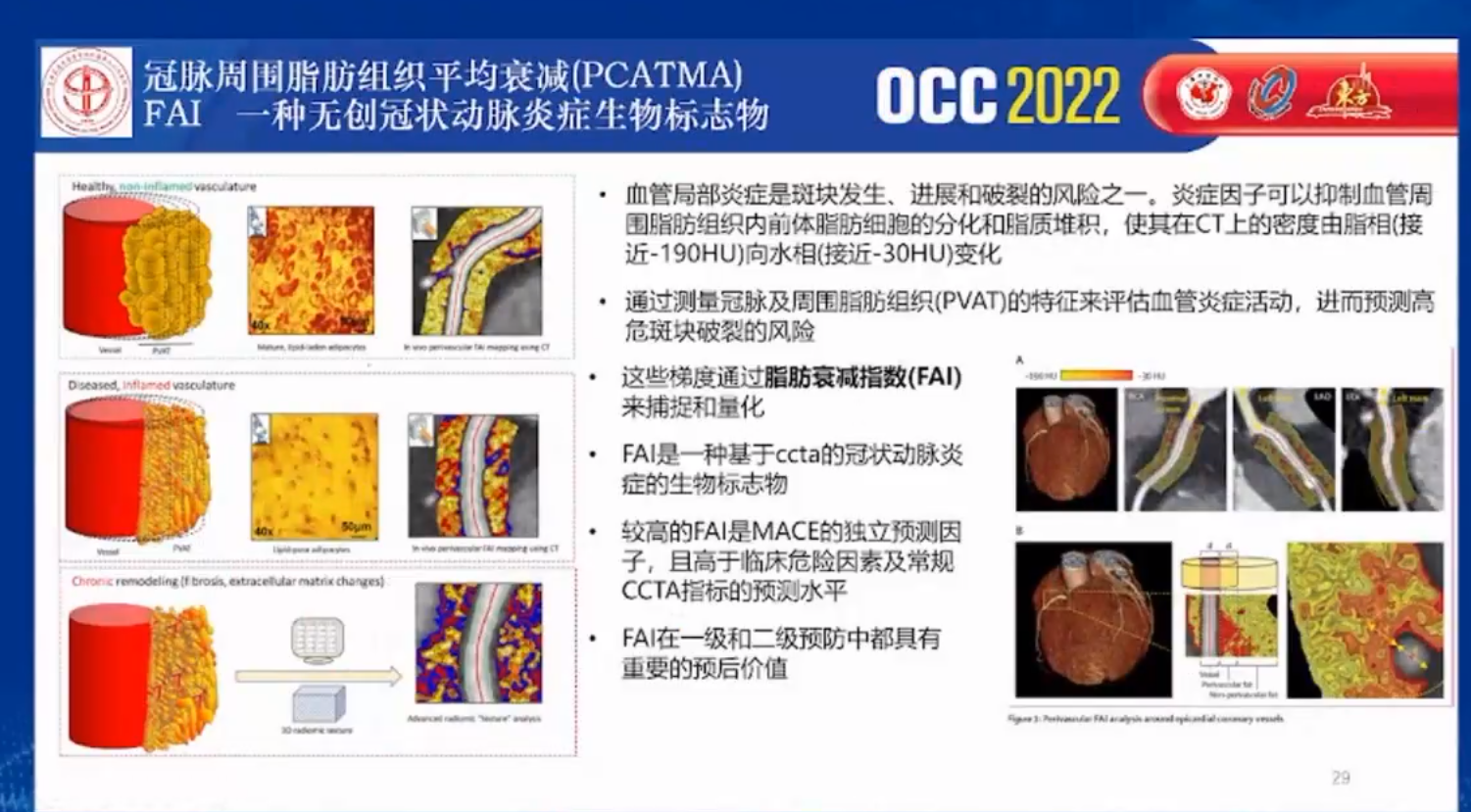
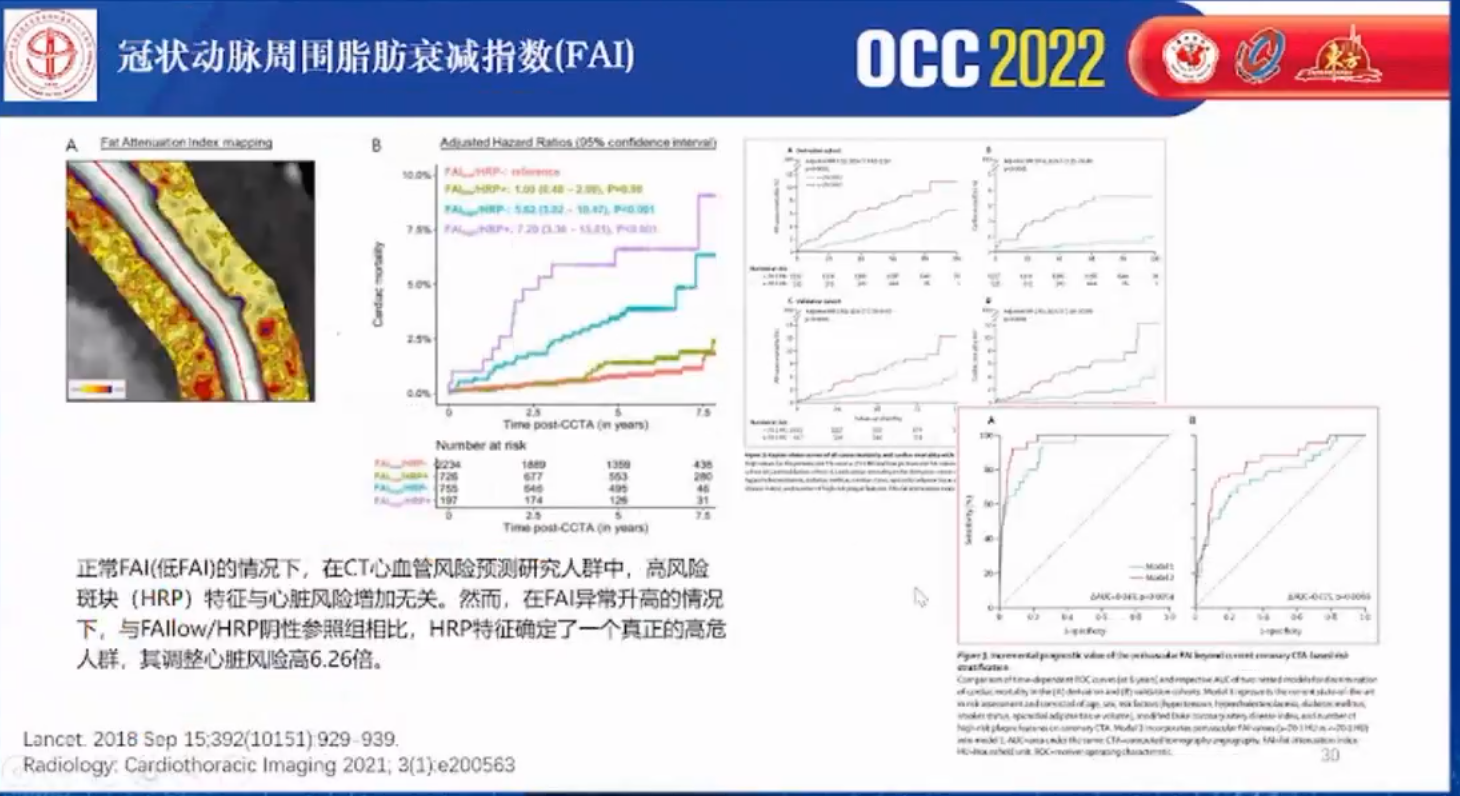
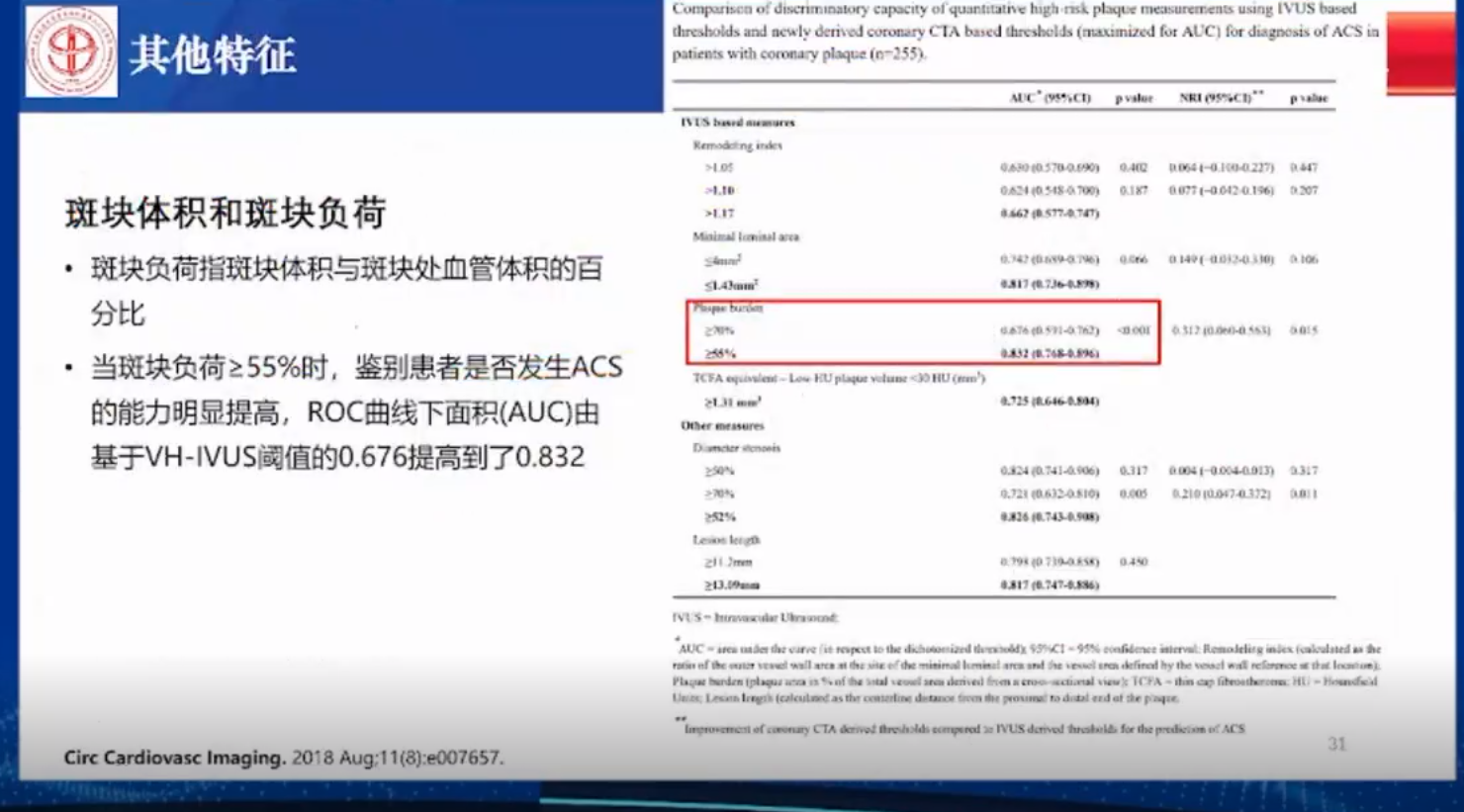
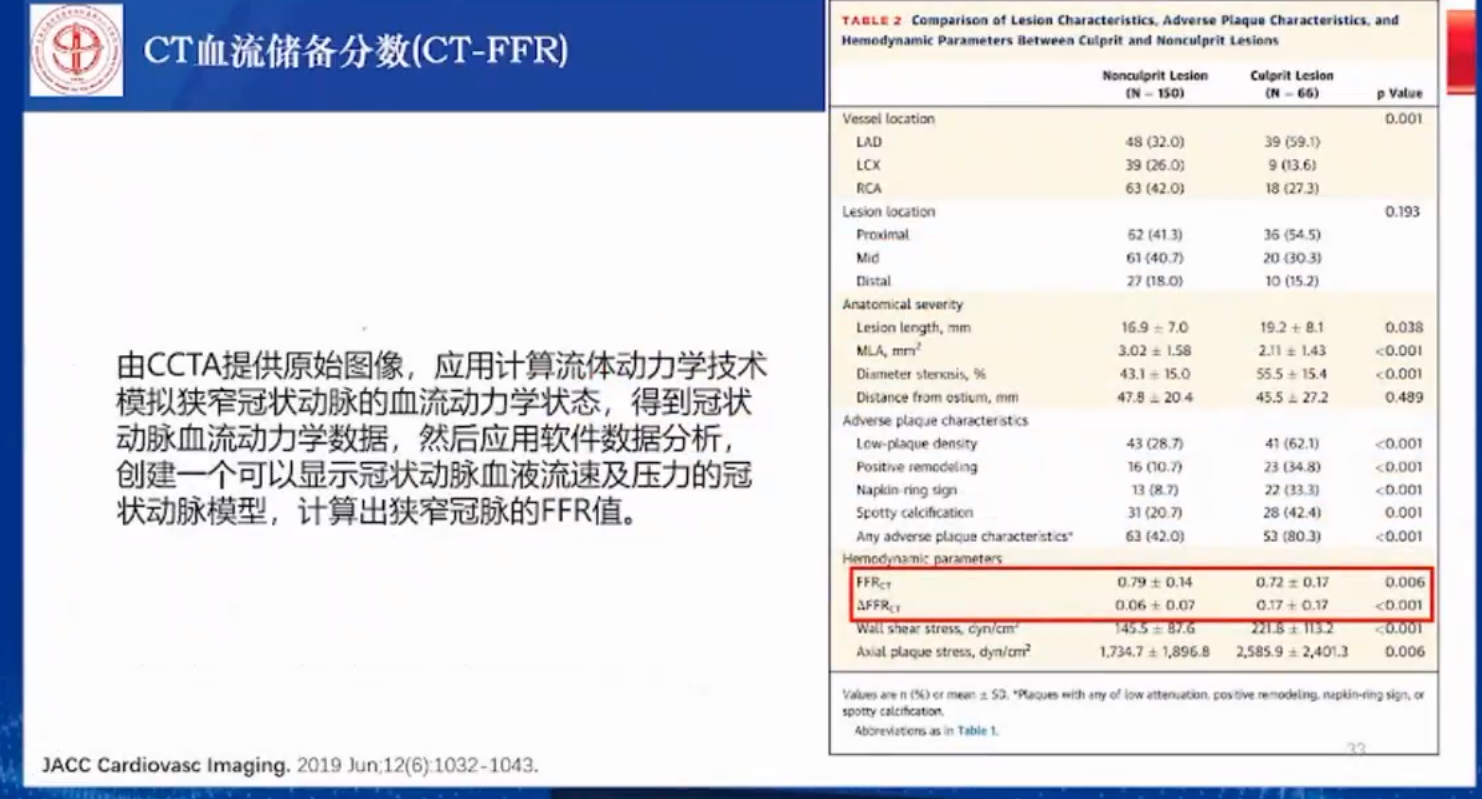
除此之外,还有关于斑块体积和斑块负荷以及CT血流储备分数等的研究。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#斑块#
52
#OCC#
0
#冠脉CT#
38
学习了
53
学习中
49