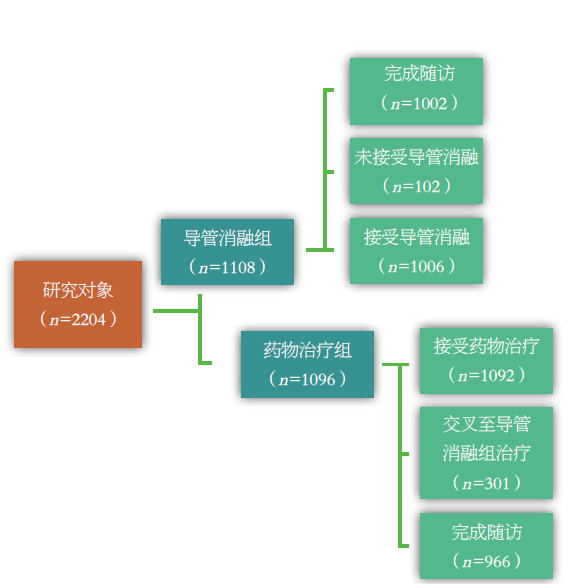
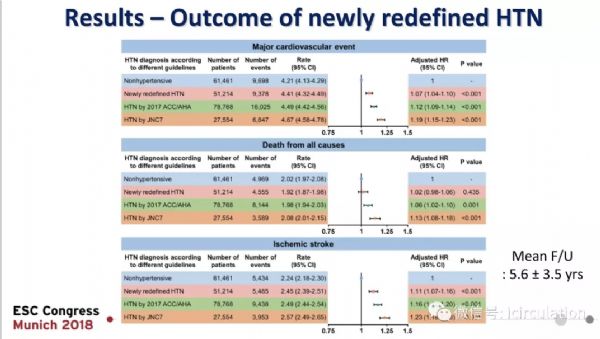
房颤治疗,选择导管消融还是药物? ——CABANA研究解读
2018-09-07 马长生 中华医学信息导报
导管消融已成为心房颤动(房颤)治疗的重要手段。目前,对于抗心律失常药物治疗无效的阵发性房颤,欧美指南均将导管消融作为Ⅰ类推荐。对于无或伴轻微心脏病的症状性阵发性房颤患者,导管消融甚至可以是经过选择的患者的初始治疗方案。


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ANA#
35
原文链接在哪里呢
93
快乐学习每一天
87
#导管消融#
45
#消融#
28
看看
88