BMJ Open:2型心肌梗死与1型心肌梗死的诊断、治疗和预后比较
2022-02-23 “心关注 ”公众号 “心关注 ”公众号
心肌梗死(MI)的临床定义随时间的推移而不断演变,在临床实践中区分2型(T2MI)和1型(T1MI)可能比较困难,且T2MI的治疗和预后仍不明确。
心肌梗死(MI)的临床定义随时间的推移而不断演变,在临床实践中区分2型(T2MI)和1型(T1MI)可能比较困难,且T2MI的治疗和预后仍不明确。为比较T2MI和T1MI的诱发因素、危险因素、治疗和结局的差异,Kyle White等人进行了一项荟萃分析,检索Medline和Embase数据库自2009年1月1日至2020年12月31日发表的所有研究并进行分析,使用纽卡斯尔-渥太华量表评估偏倚风险。

研究共纳入40项队列研究,包括98,930例T1MI患者和13,803例T2MI患者。与T1MI相比,T2MI患者更有可能存在慢性肾病(OR 1.87,95%CI 1.53-2.28)和慢性心力衰竭(OR 2.35,95%CI 1.82-3.03),不太可能出现典型的胸痛症状(OR 0.19,95%CI 0.13-0.26);更有可能出现呼吸困难(OR 2.64,95%CI 1.86-3.74);更有可能在心电图上表现出非特异性ST-T波改变(OR 2.62,95%CI 1.81-3.79),ST段抬高的可能性较小(OR 0.22,95%CI 0.17-0.28);不太可能接受冠状动脉造影(OR 0.09,95%CI 0.06-0.12)和经皮冠状动脉介入治疗(OR 0.06,95%CI 0.04-0.10)或接受心脏保护药物,如他汀类药物(OR 0.25,95%CI 0.16-0.38)和β受体阻滞剂(OR 0.45,95%CI 0.33-0.63)。T2MI1年全因死亡率风险更高(OR 3.11,95%CI 1.91-5.08),短期死亡率无显着差异(OR 1.34,95%CI 0.63-2.85)(图1)。
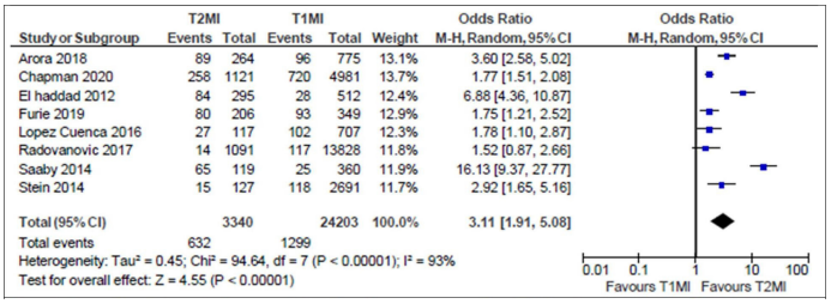
图1. T2MI和T1MI患者相比的1年全因死亡率
原始出处:
White K, Kinarivala M, Scott I. Diagnostic features, management and prognosis of type 2 myocardial infarction compared to type 1 myocardial infarction: a systematic review and meta-analysis. BMJ Open. 2022 Feb 17;12(2):e055755. doi: 10.1136/bmjopen-2021-055755. PMID: 35177458.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#BMJ#
44
#PE#
41
学习了
63
学习了
56