Behavioural Brain Research:代表性人口研究中DRD2rs6277多态性、环境和性别对冲动性的交互作用
2021-01-31 MedSci原创 MedSci原创
冲动是一种多维度的行为和人格结构,其特点是缺乏思考,倾向于进行快速、无计划的行动。冲动行为被认为是执行功能受损引起的,是功能失调的抑制过程和强烈冲动(又称欲望、冲动或习惯)的结果,由情境和性格因素触发
冲动是一种多维度的行为和人格结构,其特点是缺乏思考,倾向于进行快速、无计划的行动。冲动行为被认为是执行功能受损引起的,是功能失调的抑制过程和强烈冲动(又称欲望、冲动或习惯)的结果,由情境和性格因素触发和调节。冲动行为的倾向见于精神病态,如物质使用障碍、注意力缺陷/多动障碍(ADHD)、边缘性和反社会性人格障碍和精神分裂症。此外,情绪和行为自我控制问题是《精神障碍诊断和统计手册》中“破坏性、冲动控制和行为障碍”小节所描述的问题的核心。冲动行为可能由几种大脑神经递质系统调节,包括5-羟色胺能、去甲肾上腺素能、胆碱能和多巴胺能系统,纹状体和额叶多巴胺能异常是最常见的研究。
本研究的目的是通过进一步调查DRD2 rs6277与行为和自我报告冲动的早期逆境以及人群代表性样本中的酒精使用之间的关系,旨在探讨性别对上述结果的作用。假设作为DRD2 rs6277多态性的CC纯合子,并且在15岁前经历过大量的应激性生活事件(SLE)和/或家庭虐待导致:1)自我报告的适应不良冲动性较高,2)适应性冲动性降低,3)行为冲动性表现较差测验。其次,假设温暖的家庭关系有助于:1)较低的不适应冲动,2)较高的适应性冲动得分,3)与其他组相比,CC纯合子在行为冲动测试中表现更好。然而,由于雌激素可能提供神经保护作用,预计女性在行为和自我报告的冲动性测量中表现出的环境事件效果不如男性明显。作为第二个目的,本文探讨了DRD2 rs6277基因型与人格特质之间的关联,因为有人认为冲动性可能受到个体其他人格特质的影响。
在第一轮研究中,年轻组的平均年龄为9.6岁(SD=0.5278男性,305女性)。随访时间分别为2004年(n=483,MAge=15.3±0.5,男222,女261)、2007年(n=454,MAge=18.3±0.5,男202,女252)和2014年(n=440,MAge=25.3±0.5,男193,女247)。自适应和不适应冲动性量表(AMIS)用于测量每个研究波的冲动性自我报告方面。对378名15岁儿童进行了视觉比较试验(VCT)。基于计算机的刺激,由多个X组成的几何图形组成。该图形与另一图形配对,形成相同或不同的图形对。在同一对中,这两个数字是相同的。在不同的对中,单个X的位置在图形的外围发生了变化。
儿童和青少年系统性红斑狼疮是自我报告在15岁。系统性红斑狼疮包括21种不良经历,如父母死亡和离婚/分居、父母失业、父母双亲缺勤、经济问题、生活条件差和家庭贫困、健康状况差、慢性病、近亲死亡、家庭成员重病、家庭屈辱,对学校的恐惧和学校的欺凌。家庭关系用儿童报告塔尔图家庭关系量表进行测量,四个分量表分别测量亲密度、支持、误解和(情感和身体)虐待。由于各分量表之间的相关性,亲密度和支持度可以加在一起,形成一个更高阶的分量表,称为家庭温暖。在后续研究中,受试者报告了他们第一次饮用半单位酒精的年龄。一单位酒精被定义为一杯淡葡萄酒或香槟(12毫升)、一杯伏特加(4毫升)或一瓶(33毫升)淡酒精(啤酒、长饮、苹果酒等)。
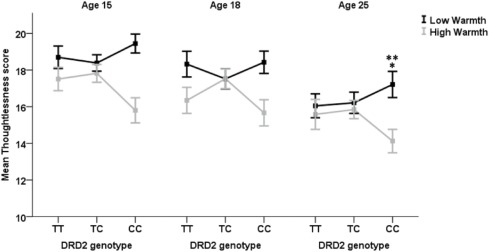
根据DRD2基因型和温暖度的中位数划分,三个研究曲线的平均无思想得分
无法确定一名参与者的基因型。总的来说,基因型分布没有偏离Hardy-Weinberg平衡(TT=157,TC=273,CC=149;X2=1.87,df=1,p=0.17)DRD2基因型与系统性红斑狼疮(SLE)发生率及家庭关系问卷评分无显著相关性(p>0.05)。也没有发现DRD2对冲动性或酒精使用测量有任何显著的主要影响。使用DRD2 rs6277基因型、性别和SLE对三个研究中自我报告的冲动性测量进行GEE分析的完整结果。GEE分析显示,在三个研究中,对无思想性的影响存在显著的三因素交互作用(χ2=5.567,p=0.062);在单独的研究中,方差分析显示,在25岁时,对无思想性的影响存在显著的三因素交互作用(DRD2×SLE×性别交互作用)。两组受试者均未发现明显的DRD2×ELS交互作用,p>0.05。在所有研究波中,DRD2×SLE对不适应冲动性的双向交互作用都有轻微的显著性(GEE;χ2=5.537,p=0.063),这种交互作用在15岁时最为明显,F(2,461)=4.760,p=0.009,部分η2=0.020,π=0.792。
在适应不良或适应性冲动综合得分上,DRD2基因型、性别和温暖没有出现显著的三方交互作用。对SST结果的分析显示,在委托误差上,DRD2×SLE的相互作用具有轻微的显著性,F(2338)=2.438,p=.089,部分η2=.014,π=.489,在SSRT上,F(2308)=2.677,p=.070,部分η2=.017,π=.529。DRD2基因型F(2,338)=2.591,p=.076,部分η2=.017,π=.515对平均Go反应时间也有微显著的主效应,CC纯合子慢于TC杂合子和TT纯合子。以DRD2基因型、系统性红斑狼疮和性别为预测变量的GEE对研究波中的饮酒频率显示出略微显著的DRD2×系统性红斑狼疮交互作用(χ2=4.971,p=0.083),以及三因素DRD2×系统性红斑狼疮×性别交互作用(χ2=5.007,p=0.082)。
这项研究表明DRD2 rs6277多态性与SLE和家庭环境在影响自我报告冲动方面相互作用,CC纯合子在不利环境中普遍表现出高度的适应不良冲动。另一方面,有一些证据表明CC携带者男性通过表现出较低水平的轻率而受益于支持性家庭关系。基因型与环境的交互作用以及与性别的进一步交互作用在饮酒习惯中也很明显。行为冲动性测试的结果显示,DRD2×SLE的相互作用仅具有轻微的显著性。
K. Klaus, M. Vaht, K. Pennington, J. Harro, Interactive effects of DRD2 rs6277 polymorphism, environment and sex on impulsivity in a population-representative study,Behavioural Brain Research,Volume 403,2021,113131,
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#HAV#
41
#互作#
40
#EHA#
36
#Research#
35
#多态性#
32
酒精貌似....仅次于烟草了
75