48岁,男性。
心肺复苏后出现管状视野。
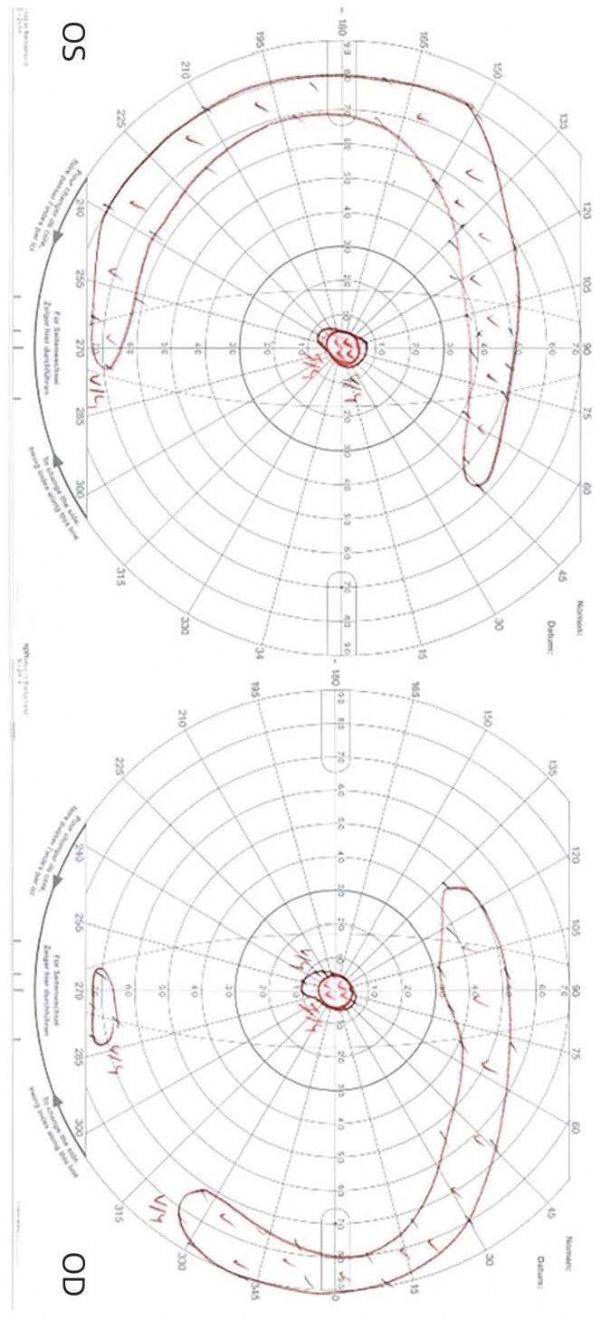
Goldmann视敏度分析显示双侧同向对称性偏盲,中心及双侧颞叶弧形视野缺损(下图)。
下图,患者心肺复苏6个月后Goldmann视野检查发现双侧中心及颞叶弧形视野缺损:
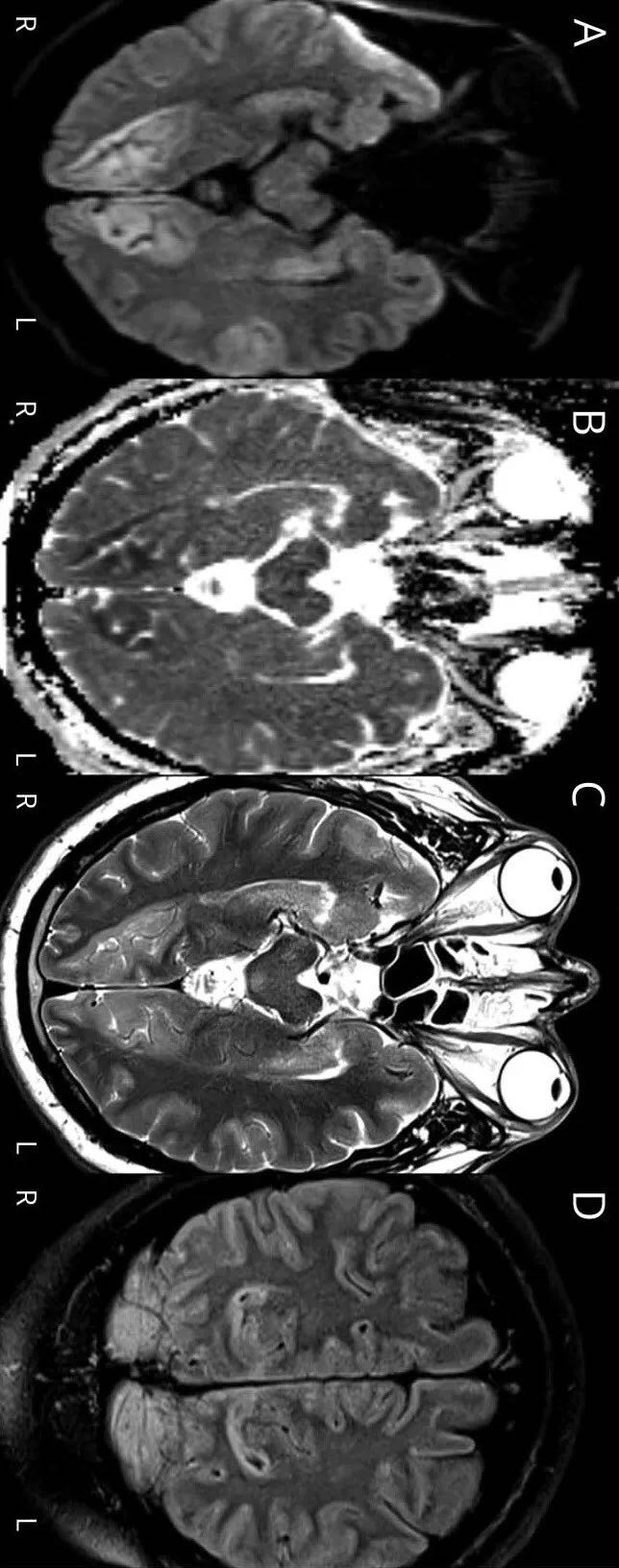
眼底检查正常,MRI显示双侧后分水岭梗死(bilateral posterior watershed infarctions)(下图)。
下图,心肺复苏3天后轴位DWI(A图)、ADC(B图)、T2(C图)和冠状位Flair(D图)MRI发现双侧距状裂皮质异常信号:
原始出处:
Daniel Josef Lindegger, et al. Mystery Case:Bilateral temporal crescent sparing after cardiac arrest. Neurology. 2018 May 29;90(22):1035-1036.doi:10.1212/WNL.0000000000005608.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Neurol#
0
#视野缺损#
33
#双侧#
36
学习了.长知识
76