NEJM:新冠肺炎疫苗对 Omicron (B.1.1.529) 变异株的防效降低,接种“第三针”刻不容缓
2022-03-08 MedSci原创 MedSci原创
在完成两剂ChAdOx1 nCoV-19或BNT162b2疫苗接种人群中,疫苗对Omicron 变异株引起的症状性疾病的保护效果有限,接种增强针可提高保护作用

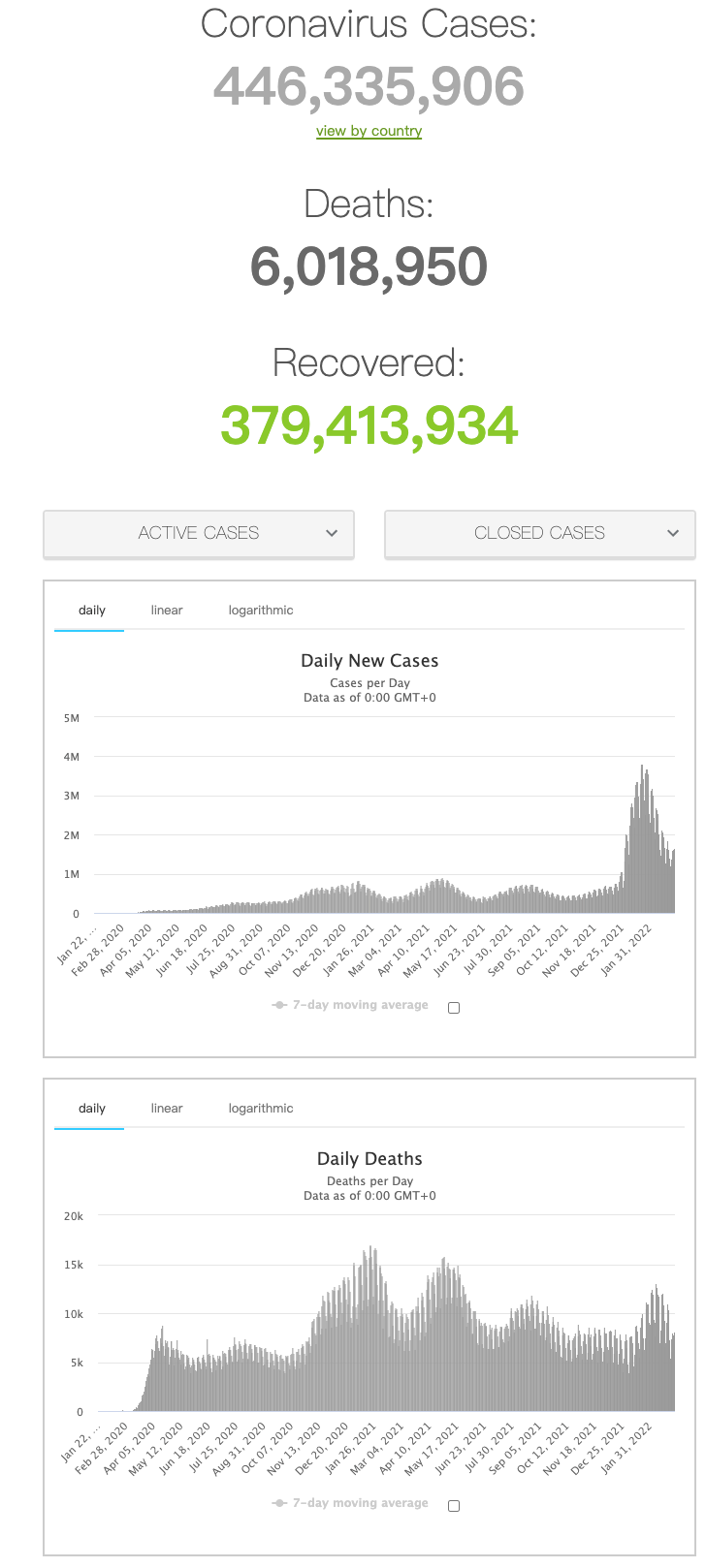
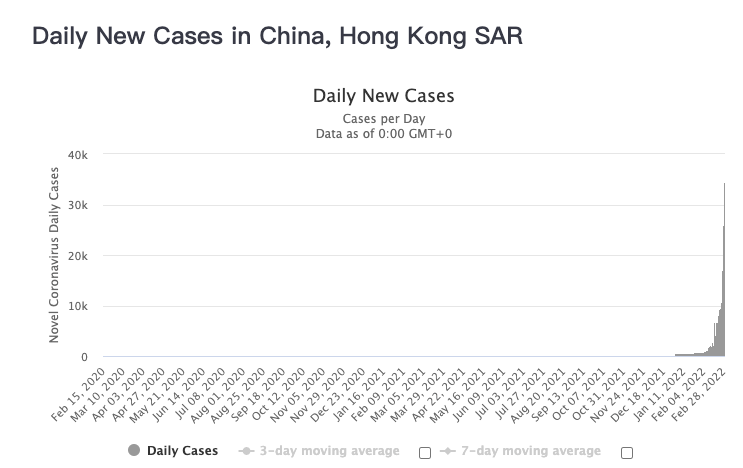
2021年11月26日,世界卫生组织SARS-CoV-2病毒进化技术咨询小组将首次在博茨瓦纳和南非发现的严重急性呼吸综合征冠状病毒2 (SARS-CoV-2) B.1.1.529变体命名为Omicron,随后Omicron成为南非新冠肺炎疫情的元凶。早期证据表明,Omicron可导致新近感染者再次感染风险增加。近日研究人员考察了mRNA疫苗对Omicron变异株的防效。
研究人员采用阴性病例对照设计来评估疫苗对英格兰Omicron和Delta(B.1.617.2)疫情的影响,参与者接种了两剂BNT162b2、ChAdOx1 nCoV-19或mRNA-1273疫苗实现了初次免疫,随后又接种了加强针。
2021年11月27日至2022年1月12日之间,共筛查出886774名OmiCon变异株感染患者,204154名Delta变体株感染患者,1572621名核酸阴性对照。所有参与者中,疫苗对预防Delta变体症状性疾病的有效性高于Omicron变体。在完成两剂ChAdOx1 nCoV-19接种后的20周内未观察到其对Omicron变异株的防效,而完成两剂BNT162b2疫苗接种后,其预防Omicron变异株导致的症状性疾病的有效性在2至4周时为65.5%,在25周或更长时间后降至8.8%。在完成2次ChAdOx1 nCoV-19接种的人群中,接种BNT162b2增强剂后2至4周,疫苗有效性增至62.4%,10周或更长时间后,疫苗有效性降至39.6%。在完成2次BNT162b2接种后,接种BNT162b2增强剂2至4周,疫苗有效性增加至67.2%,10周或更长时间后,疫苗有效性下降至45.7%。在接种mRNA-1273增强剂后2至4周,ChAdOx1 nCoV-19初始免疫人群疫苗有效性增加至70.1%,在5至9周时下降至60.9%。在BNT162b2初始免疫人群人群中,mRNA-1273增强剂在2至4周时将疫苗有效性提高到73.9%,在5至9周时,疫苗有效性降至64.4%。
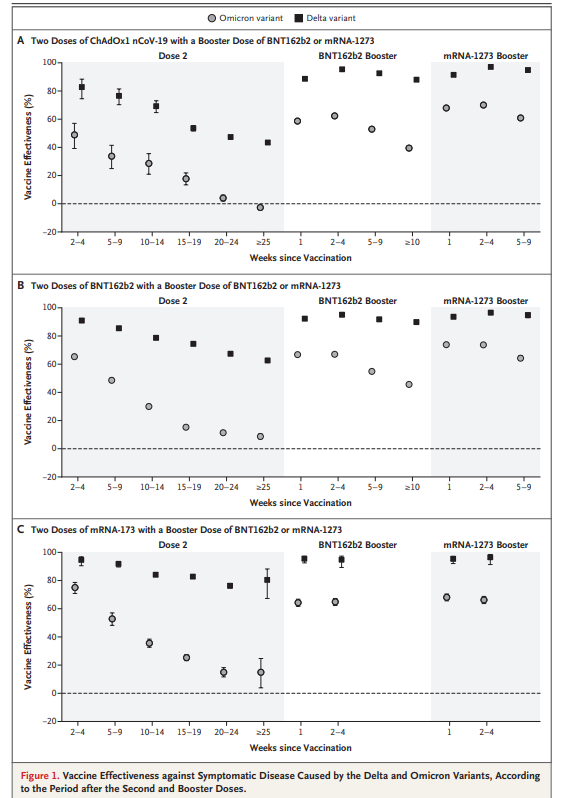
接种加强针后疫苗对 Omicron的防效增加
研究发现,在完成两剂ChAdOx1 nCoV-19或BNT162b2疫苗接种人群中,疫苗对Omicron 变异株引起的症状性疾病的保护效果有限。在完成初始免疫后,接种BNT162b2或mRNA-1273增强针可显著增加保护作用,但随着时间的推移,保护作用减弱。
原始出处:
Nick Andrews et al. Covid-19 Vaccine Effectiveness against the Omicron (B.1.1.529) Variant. N Engl J Med,March 2, 2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Micro#
56
#CRO#
37
#变异#
36
好有用哦
67