JBJS:MRI能准确评估旋后外旋型踝关节骨折的关节稳定性吗?
2015-01-16 林超文 丁香园
旋后外旋型踝关节骨折后,评估踝关节稳定性对选择手术还是保守方式非常重要。文献报道稳定性旋后外旋型踝关节骨折经保守治疗可获得满意疗效,而不稳定性旋后外旋型骨折是手术指征。 内踝和深部三角韧带是维持踝关节稳定的主要结构。深部三角韧带前束和后束主要控制距骨的旋转,但是其中一束韧带损伤后并不影响踝关节的稳定性。双踝或三踝骨折均为不稳定。然而,目前还没研究探讨内侧间隙正常情况下,单纯外踝骨折患者的
旋后外旋型踝关节骨折后,评估踝关节稳定性对选择手术还是保守方式非常重要。文献报道稳定性旋后外旋型踝关节骨折经保守治疗可获得满意疗效,而不稳定性旋后外旋型骨折是手术指征。
内踝和深部三角韧带是维持踝关节稳定的主要结构。深部三角韧带前束和后束主要控制距骨的旋转,但是其中一束韧带损伤后并不影响踝关节的稳定性。双踝或三踝骨折均为不稳定。然而,目前还没研究探讨内侧间隙正常情况下,单纯外踝骨折患者的深部三角韧带完整性与踝关节稳定性之间的关系。
既往研究表明,外旋应力试验X线平片内侧间隙≥5mm提示深部三角韧带完全断裂,需要进行手术修复或重建。临床上经常通过在透视下行外旋应力试验测量内侧间隙,从而间接评估深部三角韧带损伤程度。只有少数学者通过MRI评估深部三角韧带的完整性,判断踝关节是否稳定,来指导治疗方案的选择。
应力外旋试验的界值5mm是否能准确评估深部三角韧带损伤仍存在争议。对于应力外旋试验阳性(>5mm)而MRI只提示深部三角韧带后束部分损伤,Koval等通过保守治疗获得满意疗效。然而,目前还没有研究通过MRI评估三角韧带损伤的明确指标,而且既往研究只纳入了外旋应力试验阳性的患者。
因此,Simo Nortunen等通过MRI观察旋后外旋型踝关节骨折患者的深部三角韧带损伤情况,评估踝关节稳定性。文章最近发表在JBJS上。
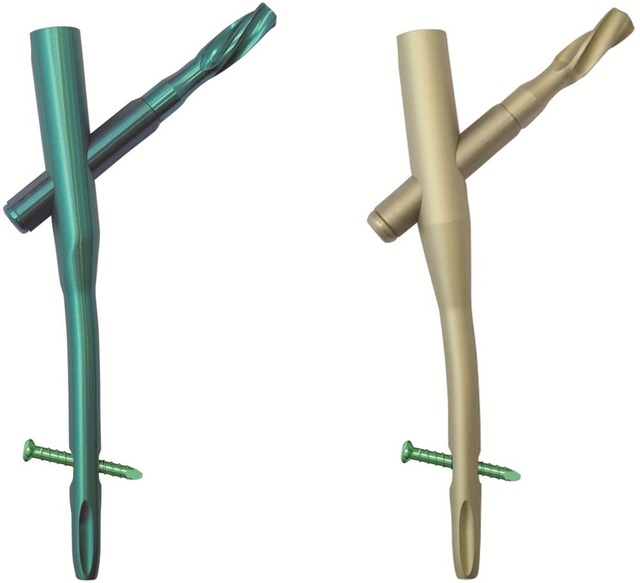
该前瞻性研究纳入61例旋后外旋型的单侧外踝骨折,由两名医生分别进行外旋应力试验评估踝关节稳定性(外旋应力试验内侧间隙≥5mm为不稳定型)(图1)。

图1:左图-外旋应力试验阴性提示踝关节稳定;右图-外旋应力试验提示踝关节不稳定。
通过3.0MRI评估深部三角韧带前束和后束损伤情况,并分为四级(正常、水肿、部分撕裂和完全断裂)(图2)。然后,比较稳定型和不稳定型踝关节的内侧间隙和MRI结果,同时还要计算外旋应力试验和MRI报告的观察者间信度。

图2:踝关节冠状位MRI图像,A-正常患者的深部三角韧带(箭头);B-深部三角韧带水肿(箭头);C-深部三角韧带部分撕裂(箭头);D-深部三间韧带完全断裂(箭头)。
有33例患者外旋应力试验内侧间隙≥5mm,而这些患者MRI结果均提示深部三角韧带损伤(5例水肿、26例部分撕裂和2例完全断裂)。还有28例患者外旋应力试验内侧间隙<5mm,MRI结果也提示深部三角韧带损伤(9例水肿和19例部分撕裂)。
one-way ANOVA提示深部三角韧带损伤越严重,内侧间隙越宽。外旋应力试验的观察者间信度高,但是MRI结果的观察者间信度一般,主要原因是即使是3.0MRI也不能发现距骨移位。
因此,作者并不推荐MRI结果作为旋后外旋型踝关节骨折治疗方案的重要参考因素。而外旋应力试验可指导临床医生决定单纯旋后外旋型外踝骨折且内侧间隙正常的患者是否需要手术治疗。
[译者注]:临床上关于外踝骨折伴三角韧带损伤的治疗一直存在争议,一部份学者认为三角韧带深层解剖位置和结构决定了它显露及处理困难,有文献结果提示损伤后通过保守治疗可自行修复,故不主张手术。
而另一部分学者认为三角韧带损伤后进入关节影响复位,且部分以瘢痕组织连接而影响愈合,往往遗留踝关节不稳、疼痛等后遗症,故三角韧带完全断裂者应手术修复,有利于早期康复和踝关节稳定。
原始出处:
Nortunen S1, Lepojärvi S1, Savola O2, Niinimäki J1, Ohtonen P1, Flinkkilä T1, Lantto I1, Kortekangas T1, Pakarinen H1.Stability assessment of the ankle mortise in supination-external rotation-type ankle fractures: lack of additional diagnostic value of MRI.J Bone Joint Surg Am. 2014 Nov 19;96(22):1855-62. doi: 10.2106/JBJS.M.01533.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









不错,赞一个
126
这篇文章有一定深度
144
是一篇不错的文章
192
非常实用
163
患OS这个疾病的高风险人群提供干预措施以避免不良预后和机械治疗措施
88
#稳定性#
25
#踝关节骨折#
37
#踝关节#
40
#JBJS#
46
学习中
70