长寿是一个异质性状,容易受到遗传和环境因素的影响。以前的全基因组关联研究(GWASs)揭示了与人类寿命或父母寿命相关的基因位点,而环境因素,包括社会经济地位、吸烟、性别和生活方式,被认为是决定因素。
观察性研究也以各种风险因素的关联为特色,其中预测的寿命可因心血管疾病(CVD)、糖尿病、高血压和吸烟而明显减少。然而,由于容易出现反向因果关系和混杂偏差,大多数流行病学研究都不足以得出明确的因果关系结论。
孟德尔随机化(MR)是一种可以克服这种局限性的分析方法,它将遗传变异作为工具变量(IVs)来评估暴露对结果的因果效应。由于基因型是由父母随机分配给后代的,在没有多态性的情况下,MR方法不太可能受到反向因果关系和测量误差的影响,与传统的研究设计相比,因果推断更加可行。
尽管一些MR分析已经证明了与长寿有因果关系的环境因素子集,但对因果暴露的探索仍处于相对原始的阶段。然而,通过应用环境流行病学领域提出的 "暴露组 "概念,我们首次能够调查影响个体从受孕到死亡的全部环境暴露。
环境因素与人类的长寿有关,但它们的特异性和因果关系大多仍不清楚。为此,来自复旦大学附属华山医院神经内科的郁金泰教授团队通过整合环境流行病学领域的创新 "暴露组 "概念,利用MR方法确定暴露组中与长寿有因果关系的成分,结果发表在BMC Medicine杂志上。
研究人员从英国生物库的361194人中提取了总共4587个环境暴露因素,评估了暴露体的外源性和内源性领域。研究了每个环境因素与两个长寿结果(即存活到第90或99百分位数的年龄)之间的关系,这些结果来自欧洲血统的不同队列。
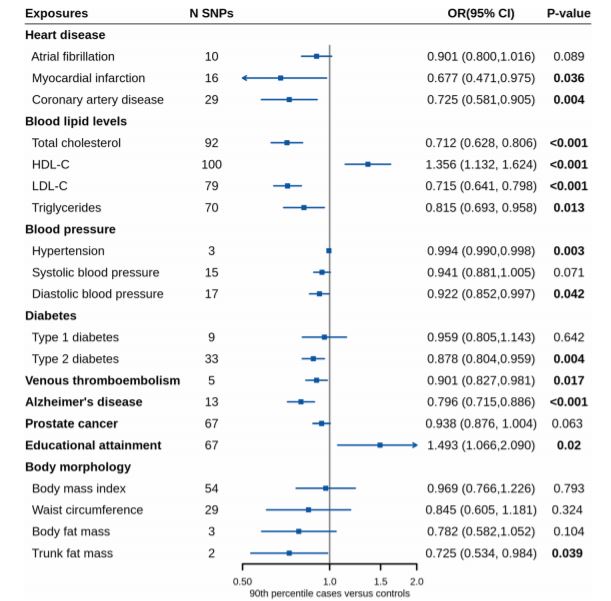
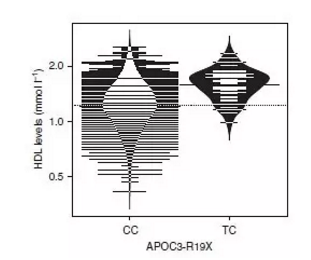
使用独立暴露GWAS进行验证的孟德尔随机化结果。
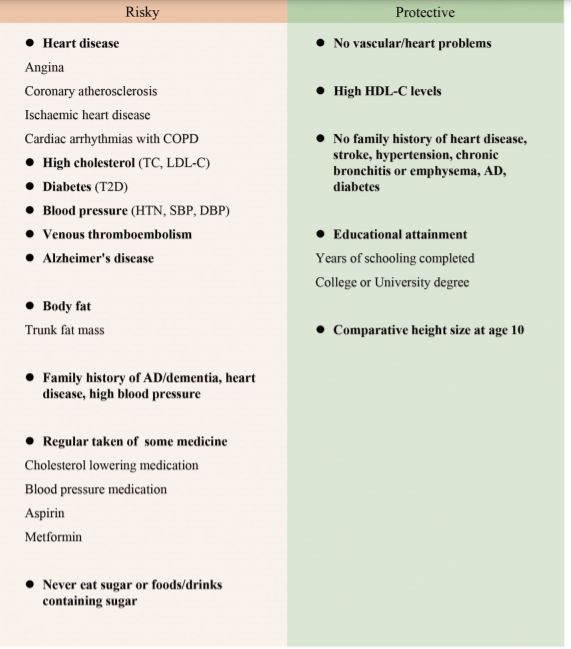
结果显示,在所有的环境暴露中,有8种与年龄有关的疾病和病理状况与较低的长寿几率有因果关系,包括冠状动脉粥样硬化(OR=0.77,95%CI:0.70,0.84)、缺血性心脏病(0.66,[0.51,0.87]),心绞痛(0.73, [0.65, 0.83]),阿尔茨海默病(0.80, [0.72, 0.89]),高血压(0.70, [0.64, 0.77])、2型糖尿病(0.88 [0.80, 0.96])、高胆固醇(0.81, [0.72, 0.91])和静脉血栓栓塞症(0.92, [0.87, 0.97])分别与降低长寿23%、34%、27%、20%、30%12%、19%和8%有关。
在调整了不同类型血脂之间的遗传相关性后,较高的低密度脂蛋白胆固醇水平(0.72 [0.64, 0.80])与较低的长寿几率有关,而高密度脂蛋白胆固醇(1.36 [1.13, 1.62])显示出相反的情况。更多的身体脂肪,特别是躯干脂肪量,以及从不吃糖或含糖的食物/饮料与长寿有不利的关系,而教育程度高则是长寿的保护因素。
对长寿的正面影响因素和负面影响因素。左侧,是对长寿有负面影响的风险因素;右侧,是对长寿有正面影响的因素
另一方面,遗传预测的坐姿/站姿身高与长寿无关。但有趣的是,10岁时较高的身高或不利于长寿。
综上,本研究结论提示与年龄有关的疾病以、教育与长寿有因果关系,并强调了实现长寿的几个新目标,包括管理静脉血栓栓塞症、适当的糖摄入和控制身体脂肪。
参考文献:
Investigating causal relationships between exposome and human longevity: a Mendelian randomization analysis. BMC Med 19, 150 (2021). https://doi.org/10.1186/s12916-021-02030-4
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#我国学者#
24
#BMC#
24
学习了~
0
#Med#
34
学习
49