Am J Clin Dermatol:IL-12/23、IL-17和IL-23抑制剂治疗银屑病的药物存活率
2022-08-25 医路坦克 MedSci原创
银屑病是一种炎症性、免疫介导性皮肤病,本文的目的是提供最新批准用于治疗中到重度银屑病的生物制剂的药物存活率的大型多中心数据,并确定可能影响这些药物药物存活率的临床预测因素。
银屑病是一种炎症性、免疫介导性皮肤病。近年来,关于银屑病发病机制的研究显著增加,由于生物制剂的高效和安全,其已经改变了对中到重度银屑病的治疗预期和目标。然而,由于治疗效果较差或发生不良事件(AEs)而中断治疗是经常发生的,通常需要更换生物制剂。
这项研究在多个国家开展,目的是提供最新批准用于治疗中到重度银屑病的生物制剂--ustekinumab, secukinumab, ixekizumab, brodalumab, guselkumab, and risankizumab的药物存活率的大型多中心数据,并确定可能影响这些药物药物存活率的临床预测因素。
方法:这项来自葡萄牙、西班牙、意大利、瑞士、捷克共和国、加拿大和美国16个皮肤科中心的多中心回顾性队列研究纳入了2012年1月1日至2019年12月31日期间开始使用IL-12/23、IL-17(IL-17A和IL-17R)和IL-23抑制剂治疗银屑病的患者。生存分析使用Kaplan-Meier估计器,以获得描述性生存曲线和比例风险Cox回归模型。
结果:共纳入3312个疗程(共3145例),其中使用IL-12/23抑制剂(Ustekinumab)1118个疗程(33.8%),使用IL-17抑制剂1678(50.7%)个疗程[Suckinumab 911(27.5%),Ixekizumab 651(19.7%),brodalab 116(3.5%)],IL-23抑制剂516(15.5%)[guselkumab 398(12.0%),risankizumab 118(3.5%)]。18个月时,risankizumab、Guselkumab、brodalab、ustekinumab、ixekizumab和secukinumab的累积生存概率分别为96.4%、91.1%、86.3%、86.1%、82.0%和79.9%。以Ustekinumab为参照物,Guselkumab的药物存活率较高(HR 0.609;95%CI为0.418~0.887),而Suckinumab的药物存活率较低(HR为1.490;95%CI为1.257~1.766)。在最终的多变量模型中,secukinumab、女性、较高的BMI和先前接触生物制剂显著增加停药风险,而risankizumab具有保护作用。
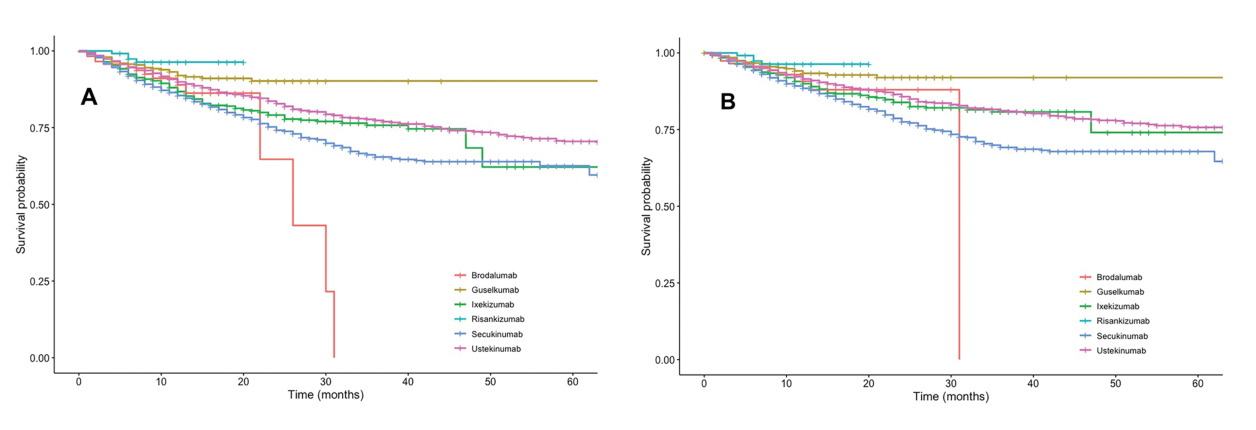
药品存活率。A总体药物存活率;B因无效而停药的药物存活率
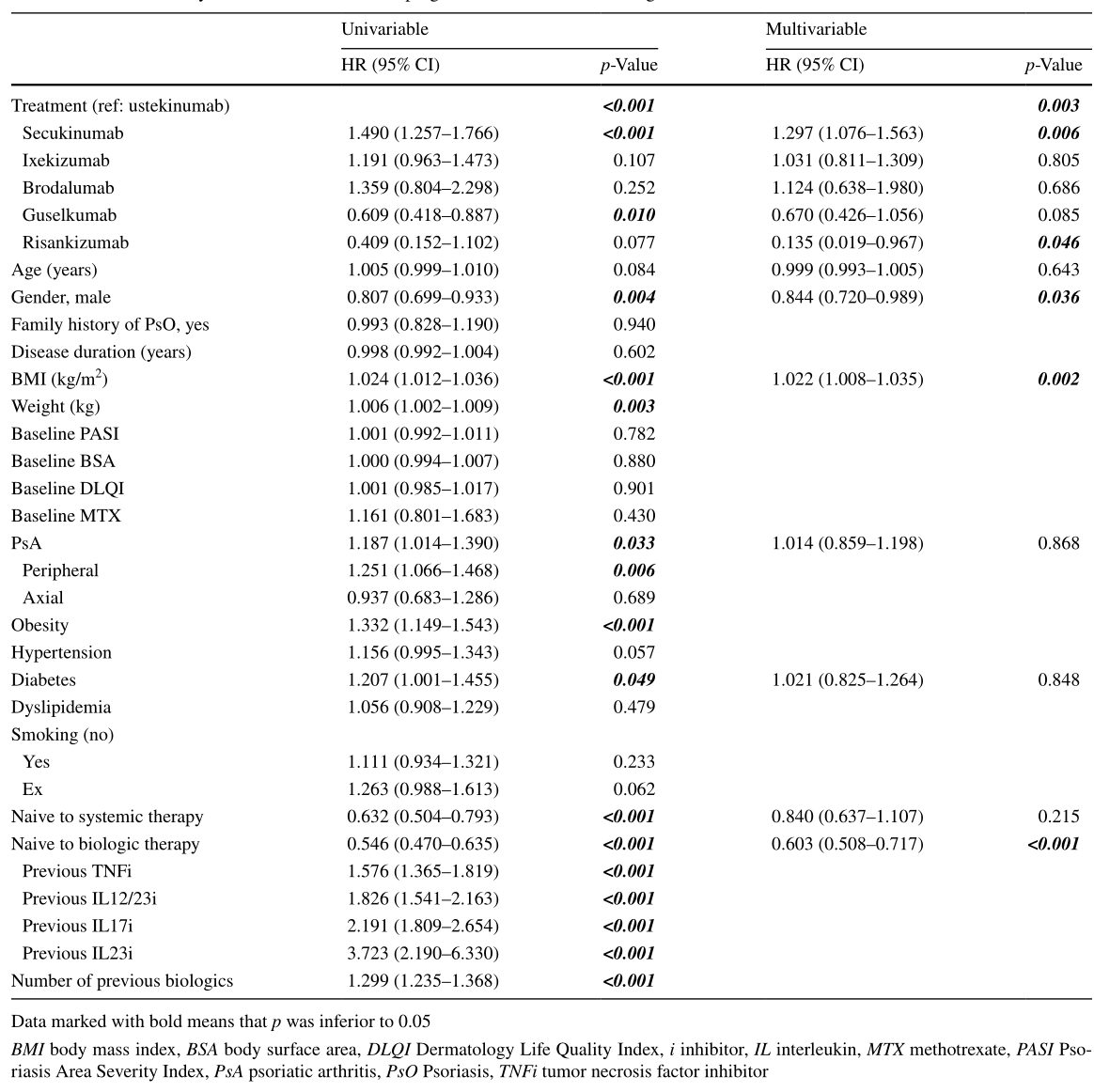
全面停药的单因素分析和最终多变量预后模型
结论:在这个有8439个病人年随访的多国队列中,所有药物在18个月时的累积存活率>79%。女性、较高的BMI和既往接触生物制剂是停药的预测因素。Guselkumab和Risankizumab的药物存活率高于Ustekinumab,Secukinumab低于Ustekinumab。
文献来源:Torres T, Puig L, Vender R,Drug Survival of Interleukin (IL)‑17 and IL‑23 Inhibitors for the Treatment of Psoriasis: A Retrospective Multi‑country, Multicentric Cohort Study.Am J Clin Dermatol 2022 Aug 17
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#抑制剂#
82
#存活率#
49
#IL-12#
44
#IL-17#
68
#IL-23#
43
#IL-1#
40
#IL-2#
57