Br J Cancer:乳腺癌中的钠离子浓度可预测肿瘤的恶性程度和治疗反应
2022-04-28 xiaozeng MedSci原创
23Na MRI成像或可作为疾病恶性程度和治疗反应的潜在的非侵入性生物标志物。
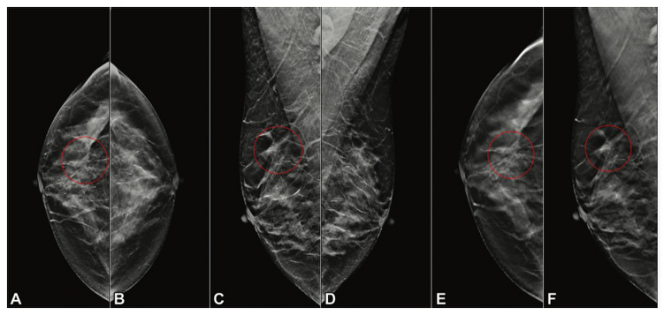
转移性乳腺癌是全球女性癌症相关死亡的主要原因之一,其中,三阴性乳腺癌亚型对应着患者较差的预后。当前该疾病的标准护理策略包括X光检查、超声、磁共振成像(MRI)和活检。在护理策略中加入额外的MRI诊断可通过早期诊断、肿瘤结构和形态的评估以及治疗反应监测来改善患者的预后。因此,迫切需要新型的非侵入性MRI生物标志物来改善患者的临床预后。

先前的研究表明,不同于传统的基于质子的成像技术,基于肿瘤内钠离子浓度(Na+)的非侵入性23Na MRI或可成为乳腺癌的生物标志物。在该研究中,研究人员旨在探索23Na MRI在乳腺癌临床前模型中的诊断和治疗监测潜力。
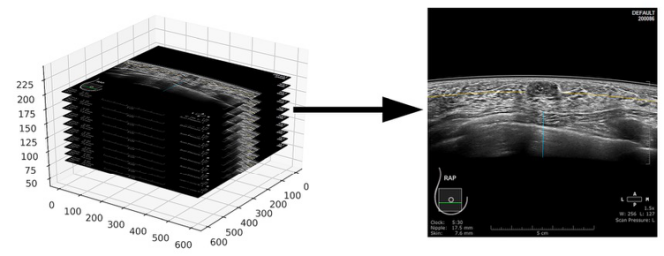
研究人员选取了携带原位乳腺肿瘤(MDA-MB-231、EMT6和4T1)的雌性Rag2-/-、Il2rg-/-和Balb/c小鼠,通过MRI、离体荧光显微镜和电生理学等技术探测相应的肿瘤生物学指标。
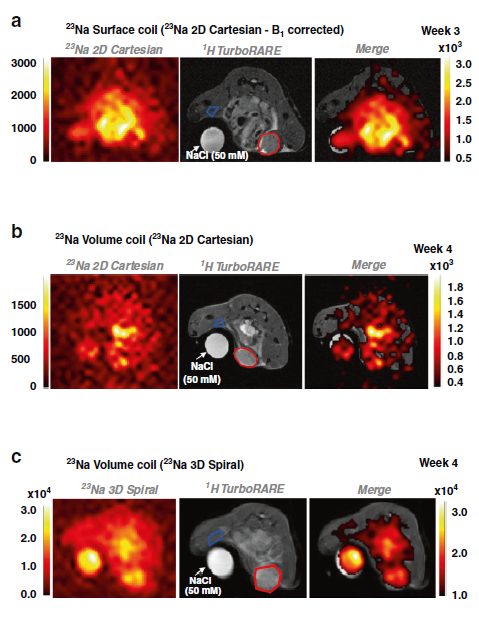
23Na MRI显示移植瘤中Na+浓度升高
23Na MRI结果显示,肿瘤中的钠离子浓度(Na+)相比于非肿瘤区域显著升高。基于互补质子的扩散加权成像(DWI)可将肿瘤中升高的Na+与相应的细胞结构进行关联。与单独使用上述任一参数相比,结合23Na MRI和DWI的成像技术能够实现肿瘤与非肿瘤区域极佳的分类精度。
进一步的研究显示,离体肿瘤切片评估证实细胞内Na+浓度升高,而细胞外则保持不变。使用特异性Na+交换抑制剂(卡立泊来德cariporide、醋酸艾司利卡西平eslicarbazepine acetate)治疗并不能影响肿瘤内的Na+浓度。尽管如此,研究人员发现,多西紫杉醇(docetaxel)能够有效的减少肿瘤中的Na+浓度,但DWI的测量值并无显著变化。
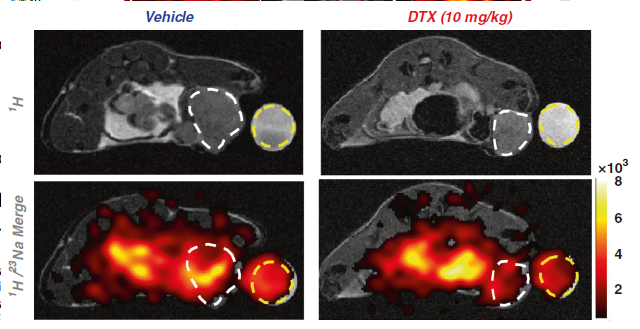
多西紫杉醇降低移植瘤中最大23Na信号
总而言之,该研究结果显示,在原位乳腺癌模型中能够检测到异常升高的Na+浓度。此外,23Na MRI成像技术能够增强DWI的诊断能力,且具有更高的灵敏度,其或可作为疾病恶性程度和治疗反应的潜在的非侵入性生物标志物。
原始出处:
James, A.D., Leslie, T.K., Kaggie, J.D. et al. Sodium accumulation in breast cancer predicts malignancy and treatment response. Br J Cancer (25 April 2022).
https://doi.org/10.1038/s41416-022-01802-w.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#钠离子#
50
感谢
53
#浓度#
54
学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
76
好文章,值得一读。
0