Curr Opin Ophthalmol:眼睛及附属器官中的IgG4相关疾病综述!
2017-09-02 cuiguizhong MedSci原创
加拿大多伦多大学眼科与视力科学系的Derzko-Dzulynsky L近日在上发表了一篇综述文章,重点对自2016年以来发表的研究性文章进行总结,系统性的介绍了眼窝和眼内IgG4相关的眼科疾病(IgG4-ROD)。
加拿大多伦多大学眼科与视力科学系的Derzko-Dzulynsky L近日在上发表了一篇综述文章,重点对自2016年以来发表的研究性文章进行总结,系统性的介绍了眼窝和眼内IgG4相关的眼科疾病(IgG4-ROD)。
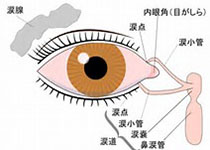
IgG4相关疾病是一种相对较新描述的多器官纤维化炎症,其组织病理学特征是淋巴浆细胞浸润,IgG4 阳性的浆细胞增加和IgG4 / IgG比例升高,超过> 40%。泪腺是最常见的眼部发病部位。近来已经报道了一些与IgG4相关的眼科疾病(IgG4-ROD),如巩膜炎和眼内炎症。在这篇综述中,作者重点对自2016年以来发表的研究性文章进行总结,系统性的介绍了眼窝和眼内IgG4相关的眼科疾病(IgG4-ROD)。
自2012年以来,有诸多研究对IgG4相关的眼科疾病,如巩膜炎和葡萄膜炎的病例进行了报告。推荐使用全身强的松作为一线治疗的方案,但对类固醇不敏感或类固醇耐药的病例可能需要进行免疫抑制治疗。在双侧IgG4-ROD患者中,全身IgG4-RD占比高,或者累及泪腺。另外,研究者指出利妥昔单抗是具有较高缓解率的最具特异性的免疫靶向治疗的药物。
因此,作者认为,IgG4相关的眼科疾病(IgG4-ROD)是巩膜炎和葡萄膜炎的发病的新的原因,应在任何患有多系统炎症性疾病的患者中进行考虑。新的靶向免疫治疗可能会是一个很好的治疗方法,能够缓解临床症状。这项工作促进了眼科临床医生完善对巩膜炎和葡萄膜炎的治疗。
原文出处:
Derzko-Dzulynsky, L., IgG4-related disease in the eye and ocular adnexa. Curr Opin Ophthalmol, 2017
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#IgG4#
41
#THA#
46
#IgG4相关疾病#
33
#IgG#
33
学习了谢谢分享
77