JACC:直立式潮式呼吸对心衰患者预后的影响
2020-06-15 MedSci原创 MedSci原创
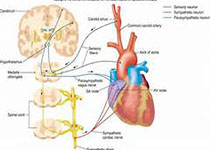
潮式呼吸(CSR)被认为仅会出现在仰卧和睡眠状态,因此,CSR治疗只适用于那些特定的状态,虽然CSR也被报道发现在清醒状态下心力衰竭(HF)患者,但它在直立位置的持续性尚不清楚。本研究的目的是评估直立
潮式呼吸(CSR)被认为仅会出现在仰卧和睡眠状态,因此,CSR治疗只适用于那些特定的状态,虽然CSR也被报道发现在清醒状态下心力衰竭(HF)患者,但它在直立位置的持续性尚不清楚。本研究的目的是评估直立CSR的预测因子、临床相关性和预后价值。
本研究纳入分析了门诊574名收缩性心衰的患者(左室射血分数是32 ± 9%,平均年龄是65 ± 13岁,男性占80%)。其中34%的患者仅表现为仰卧位的潮式呼吸,14%的患者表现为仰卧位和直立位的潮式呼吸,52%的患者呼吸方式正常。直立型CSR患者的呼吸暂停低通气和中枢性呼吸暂停指数最高(白天和夜间),血流动力学和运动能力最差,血浆去甲肾上腺素和N-末端前-B型利钠肽升高,对高碳酸血症的化学敏感性更高,而这是直立型CSR的唯一独立预测因子。经过8年时间的随访,有直立式潮式呼吸的患者预后最差,且可独立预测患者的心源性死亡风险。
研究结果显示,心衰患者直立的CSR可通过对高碳酸血症的化学敏感性增高来预测,并且与更糟糕的临床预后和更大的心脏死亡风险相关。
原始出处:
Alberto G et al.Upright Cheyne-Stokes Respiration in Patients With Heart Failure.JACC.2020 June.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#潮式呼吸#
26
#患者预后#
29
#JACC#
0
#ACC#
28
#心衰患者#
28