JACC子刊:冠脉迂曲病变可增加支架置入术后心血管事件死亡率!
2021-03-02 MedSci原创 MedSci原创
近期发布于JACC子刊上的一篇报道发现冠脉迂曲病变可增加心血管事件死亡率!
冠脉迂曲是一种常见的冠脉造影表现,与球囊血管成形术后早期和晚期主要不良事件的发生率增加有关,但是冠状动脉迂曲对于支架置入术后的临床结果的影响鲜有研究,近期发布于JACC子刊上的一篇报道发现冠脉迂曲病变可增加心血管事件死亡率!
该研究纳入6项前瞻性随机对照试验患者的资料,分析不同形态的冠状动脉病变在支架植入术后30天和5年的结果,根据冠脉是否为中度/重度迂曲病变进行分组,主要终点是靶血管衰竭(TVF;心血管相关性死亡、TV-MI:靶血管相关心肌梗死、ID-TVR:靶血管血运重建),研究共纳入6951例患者中,其中729例(10.5%)冠脉为中、重度迂曲病变并行支架植入术。
在30天时,冠脉中/重度迂曲病变患者中TVF更常见(3.8% vs 2.4%,风险比:1.64,95%CI:1.09-2.46;p=0.02),这一差异是由冠脉中/重度迂曲病变患者中TV-MI的较高导致。
5年后,由于冠脉中/重度迂曲病变患者中TV-MI(P=0.003)和ID-TVR(P=0.003)较高的发生率,冠脉中/重度迂曲病变患者的TVF仍较高(p=0.003)。
另外冠脉中/重度迂曲病变患者与无中度/重度迂曲病变的患者相比,支架内血栓发生率也更高(1.9% vs 1.0%,风险比:1.86,95%CI:1.02-3.39;p=0.04)。调整基线协变量后,5年后中度/重度血管迂曲病变患者与TV-MI和ID-TVR独立相关(p=0.04)。
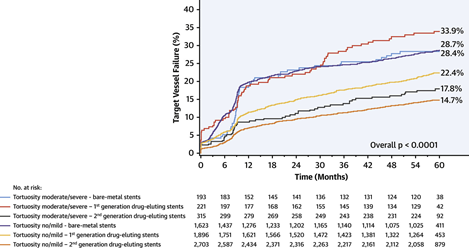
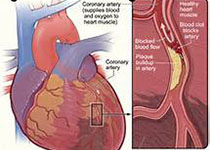
冠脉迂曲病变TVF发生率
总的来说在冠状动脉中、重度迂曲病变的血管中植入支架与心血管事件死亡率增加有关,且是由靶血管相关心肌梗死和靶血管血运重建的发生率增高导致的。
原始出处:
Konigstein M, Ben-Yehuda O, Redfors B, Mintz GS, Madhavan MV, Golomb M, McAndrew T, Zhang Z, Kandzari DE, Hermiller JB, Leon MB, Stone GW. Impact of Coronary Artery Tortuosity on Outcomes Following Stenting: A Pooled Analysis From 6 Trials. JACC Cardiovasc Interv. 2021 Feb 20:S1936-8798(20)32505-X. doi: 10.1016/j.jcin.2020.12.027. Epub ahead of print. PMID: 33640388.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#置入术#
38
学习了
52
学习了,谢谢
49
#JACC#
21
#血管事件#
20
学习了,谢谢分享
71
增加支架植入术后心血管事件的死亡率
61
#ACC#
27
好文章!
62