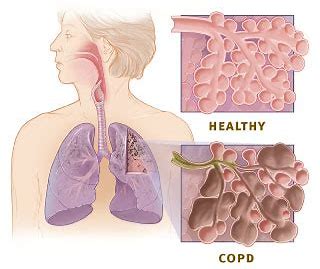
Chest:COPD患者**端粒长度与生活质量、急性发作和死亡率之间的关系
2018-07-16 xing.T MedSci原创
由此可见,这些数据表明复制性衰老可能有助于预测COPD的不良预后。较短的白细胞端粒长度作为临床生物标志物可用于确定COPD临床结局较差风险增加的个体。
COPD是一种与年龄有关的疾病。细胞衰老在COPD中的作用尚未完全阐明。近日,呼吸领域权威杂志chest上发表了一篇研究文章,该研究旨在评估了外周血白细胞端粒长度与临床结局之间的关系,包括COPD患者的健康状况、急性发作率和死亡风险。
研究人员使用定量聚合酶链反应测量了576名中度至重度COPD患者的血液样本中提取的DNA的绝对端粒长度(aTL),这些患者来自于大环内酯类阿奇霉素预防COPD恶化(MACRO)研究,并采用阿奇霉素或安慰剂治疗12个月。所有参与者随访了大约13个月,在此期间研究人员仔细确定了受试者的健康状况和恶化情况,以及29个月的死亡率。研究人员使用中值作为截止值将aTL分成两组,来确定急性发作率和死亡率。
端粒长度较短的参与者健康状况较差,其由较高的圣乔治呼吸问卷评分(β=-0.09,P=0.034)来定义。在该研究的安慰剂组中,较短的端粒组急性发作率(比值比为1.50; 95%CI为1.16-1.95; P=0.002)和死亡风险(风险比为9.45; 95%CI为2.85-31.36; P=0.015)显著高于较长的端粒组;而在阿奇霉素组中未观察到这些差异(对于急性发作的相互作用P=0.008,对于死亡率的相互作用P=0.017)。
由此可见,这些数据表明复制性衰老可能有助于预测COPD的不良预后。较短的白细胞端粒长度作为临床生物标志物可用于确定COPD临床结局较差风险增加的个体。
原始出处:
Minhee Jin,et al. Relationship of Absolute Telomere Length With Quality of Life, Exacerbations, and Mortality in COPD.chest.2018. https://doi.org/10.1016/j.chest.2018.05.022
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Chest#
20
#EST#
25
#端粒长度#
40
#COPD患者#
24
#急性发作#
22
了解一下.谢谢分享!
45