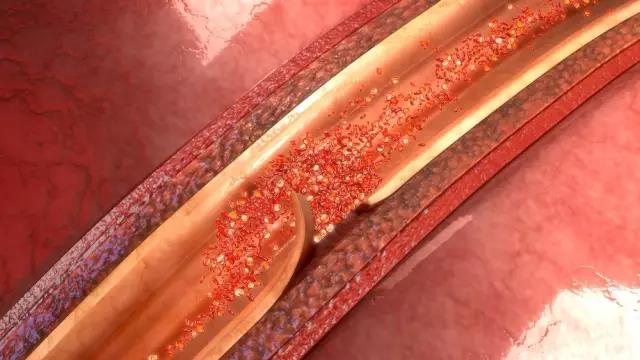
Neurology:动脉闭塞独立预测颈动脉夹层患者的不良结果
2019-11-25 xing.T MedSci原创
由此可见,DAO可独立预测CeAD患者较差的功能结局。特别是对于DAO患者,有必要进一步研究血管通畅性、侧支状态和血运重建疗法的效果。
近日,神经病学领域权威取杂志Neurology上发表了一篇研究文章,研究人员旨在评估动脉夹层闭塞(DAO)对颈动脉夹层(CeAD)患者的功能结局和并发症的影响。
研究人员分析了3个中心连续就诊的CeAD患者(颈动脉夹层和缺血性卒中[CADISP]–Plus财团数据集)的综合患者数据,纳入了具有DAO和功能结局数据的患者。研究人员将DAO患者与非DAO患者进行了比较。该研究的主要结果是从基线开始3到6个月测得的良好功能性结局(即改良的Rankin量表[mRS]评分0-1)。次要结局包括迟发性脑缺血、大出血、CeAD复发和死亡。研究人员进行了单变量和多变量二元logistic回归分析,并计算了包含95%置信区间(CI)的比值比(OR),并对潜在的混杂因素进行了调整。
2148例患者(中位年龄为45岁[四分位间距(IQR)为38-52],43.6%为女性)中,728人(33.9%)患有DAO。DAO患者更常出现脑缺血(84.6% vs. 58.5%,p<0.001)。与没有DAO的患者相比,DAO患者不太可能获得良好的结局(mRS为0-1:59.6% vs. 80.1%,调整后的P<0.001)。在调整了年龄、性别和初始卒中严重程度后,DAO与不良预后独立相关(mRS为0–1:OR为0.65,95%CI为0.50–0.84,p=0.001)。DAO患者迟发性脑缺血比无DAO的患者更常见(4.5% vs. 2.9%,p=0.059)。
由此可见,DAO可独立预测CeAD患者较差的功能结局。特别是对于DAO患者,有必要进一步研究血管通畅性、侧支状态和血运重建疗法的效果。
原始出处:
Christopher Traenka,et al.Artery occlusion independently predicts unfavorable outcome in cervical artery dissection.Neurology.2019.https://doi.org/10.1212/WNL.0000000000008654
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#颈动脉#
47
#颈动脉夹层#
46
#动脉闭塞#
34
#Neurol#
36
#动脉夹层#
39