肺结节抗炎后不吸收就建议切除?
2021-08-24 肺结节前沿 肺结节前沿
46男性,不吸烟。因感冒发热,做CT检查发现肺实性结节1.6cm。用了头孢加左氧消炎7天后,复查CT检查没有变化,当地继续予莫西沙星抗炎治疗中。
46男性,不吸烟。因感冒发热,做CT检查发现肺实性结节1.6cm。用了头孢加左氧消炎7天后,复查CT检查没有变化,当地继续予莫西沙星抗炎治疗中。
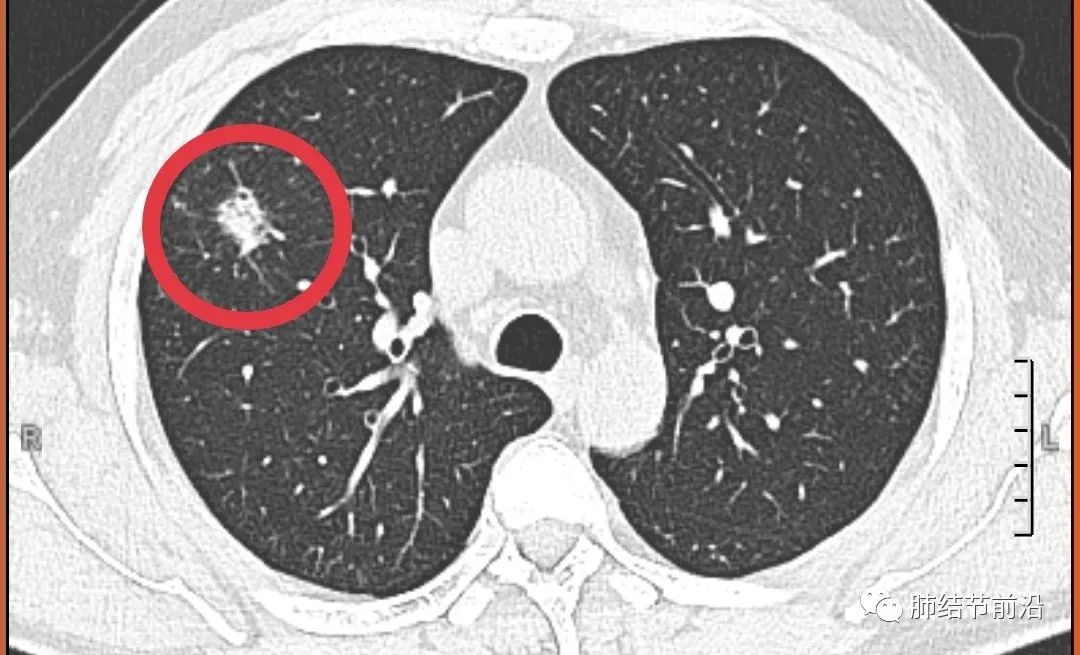
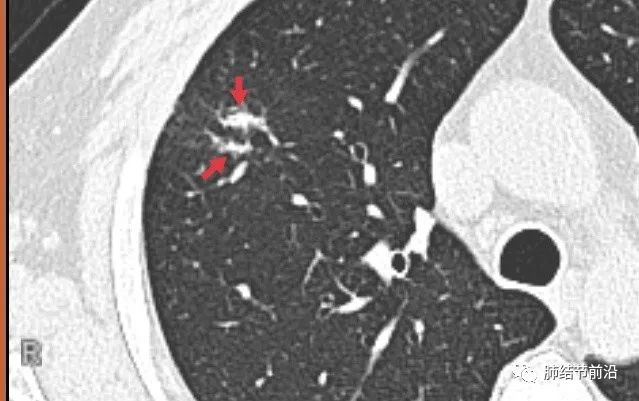
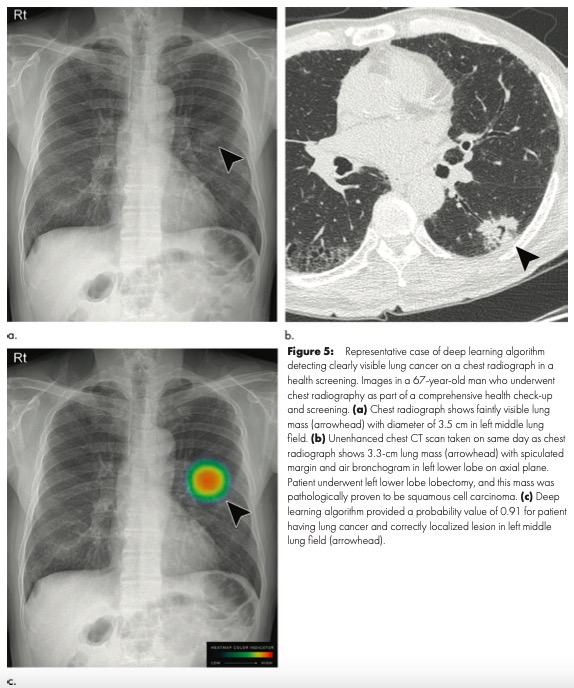
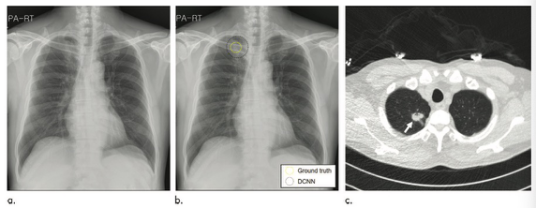
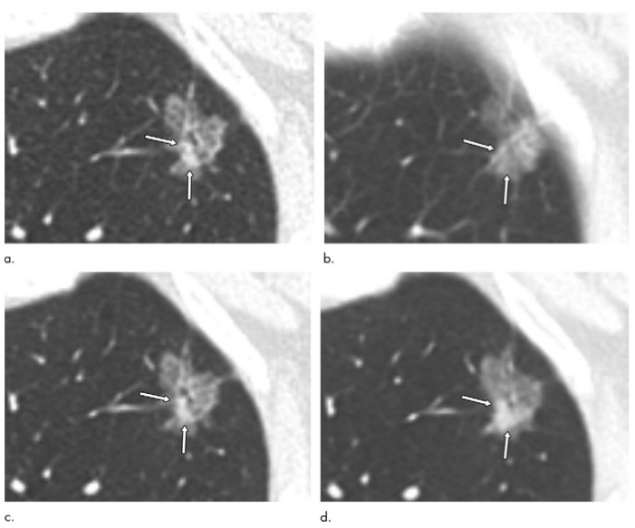
下图为首次抗炎后复查后的CT:为右上肺实性结节16mm。
由于抗炎后不吸收,有医生建议直接手术切除。
对于这种先切除再诊断再治疗的观念,窃以为极不可取。就算是微创楔形切除,毕竟也是切除了一小部分肺。只有极少数高危结节,其他方式无法确诊的情况下,才能考虑不管良恶性,切除后再诊断。
抗炎后不吸收,就要怀疑恶性,要切除吗?
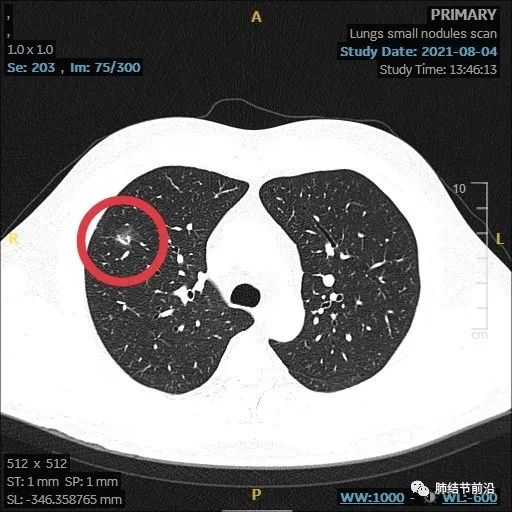
观看CT这个结节还是典型的炎症性表现,符合普通细菌性炎症,仔细再看一下结节形态:
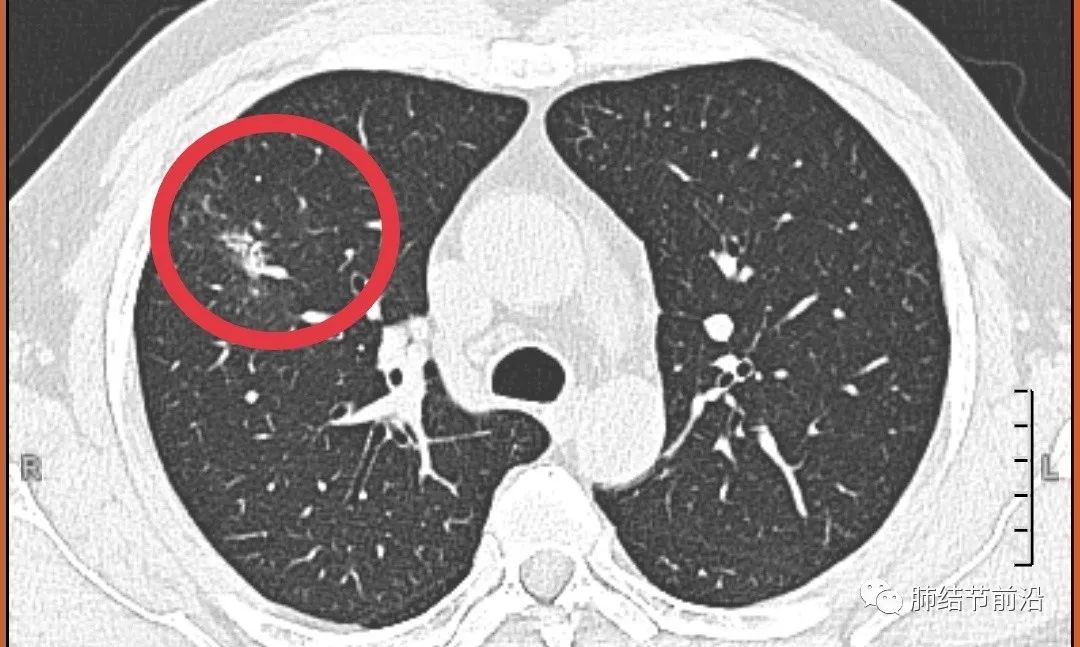
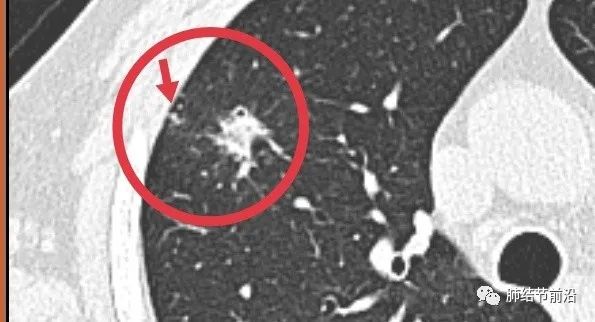
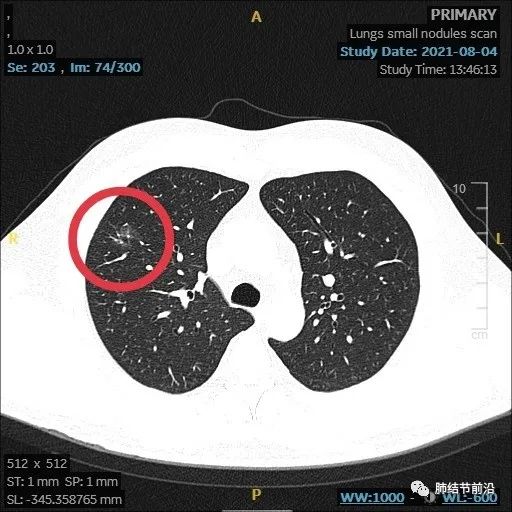
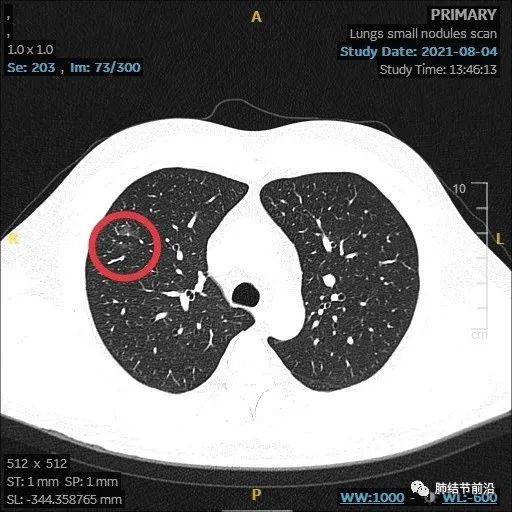
结节周围有斑点,符合炎症的表现:
结节较为分散,同样为炎症样表现:
另外,之前抗炎后复查时间太短(7天),炎症也可能不会吸收明显。而且,对于这种社区性肺部感染,选择莫西沙星或者奈诺沙星,是比头孢和左氧氟沙星更好的抗炎药物选择。
由于CT图像为典型炎症样表现炎症,没有建议患者做肿瘤标志物等进一步的血液检查,也不用做PET。
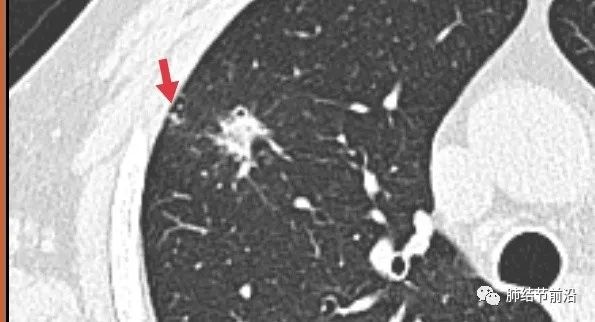
抗炎结束,后续1个月复查,结节明显吸收变淡,遗留磨玻璃影,这个磨玻璃,只是个炎症的吸收过程。而且形态上,这个磨玻璃边界不清,同样只是炎症的吸收过程。

来源:肺结节前沿
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









就一例有一般性意义吗
69
学习了
47
很好的经验
57
学习了。
64
病例很精彩,分析很全面
1
学习了,获益匪浅
49