Cancer Med:肺动脉高压是新诊断多发性骨髓瘤患者的不良预后因素
2022-05-11 网络 网络
多发性骨髓瘤(MM)仍然是一种以浆细胞克隆增殖为特征的造血恶性肿瘤。随着MM治疗的进展,包括大剂量化疗后的自体造血干细胞移植(ASCT) 、免疫调节药物、蛋白酶体抑制剂和单克隆抗体,都显著延长了患者的
多发性骨髓瘤(Multiple Myeloma,MM)是最常见的血液系统恶性肿瘤之一,以浆细胞克隆性增殖为特征,通常表现为贫血、高钙血症、骨损伤和肾功能不全。肺动脉高压 (PH) 是多发性骨髓瘤 (MM) 患者常见但很少被认可的合并症,而其对 MM 的预后意义却鲜有报道。因此,这项研究旨在评估新诊断 MM (NDMM) 患者超声心动图定义的 PH 的临床特征和预后价值,并探索潜在机制。 研究共招募了2014年1月-2020年12月期间首次确诊的北京朝阳医院(中国北京)的 426 名有症状的 MM 患者。在接受抗骨髓瘤治疗之前,患者需要在 MM 诊断时获得可用的基线超声心动图结果。诱导方案包括基于硼替佐米的方案(n = 285)、基于来那度胺的方案(联合或不联合硼替佐米,n = 110)、基于艾沙佐米的方案(n = 1)、基于达雷妥尤单抗的方案(n = 4)和传统方案化疗方案(n = 26)。145 名患者接受了自体干细胞移植(ASCT)
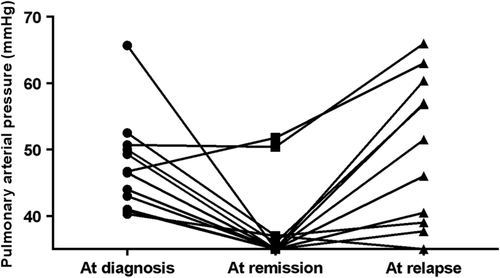
图1:不同疾病状态下的肺动脉压 (PAP)
在 12.7% (54/426) 的 NDMM 患者中发现超声心动图定义的 PH,与年龄较大、贫血和肾功能不全,以及严重的舒张功能障碍和更高的 BNP 和 NT-pro-BNP 水平相关。PH 患者的房颤发生率较高,而血栓形成的发生率与非 PH 患者相似。基于相似的治疗方案和自体干细胞移植(ASCT)率,无 PH 的患者比有 PH 的患者有更深和更好的反应(p = 0.002)。随着 MM 的缓解,81.5% 的 PH 是可逆的,伴随着右心室功能障碍的改善和 BNP/NT-pro-BNP 水平的正常化,而在 MM 复发时可能会再次发生。
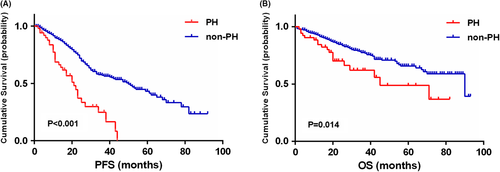
图2:PH 对无进展 (PFS) (A) 和总生存期 (OS) (B) 的影响
生存分析显示,PH 是一个不良预后因素,与无进展生存期 (PFS) (21 与 50 个月,p < 0.001) 和总生存期 (OS) (45 与 90 个月,p = 0.014) 降低相关。多变量分析进一步证实基线 PH 是较短 PFS 和 OS 的独立预测因子。
总之,超声心动图定义的 PH 是 MM 患者的不良预后指标,应在诊断时对 MM 患者进行常规评估,以做出准确的预后。
原始出处:
, , , et al. Echocardiography-defined pulmonary hypertension is an adverse prognostic factor for newly diagnosed multiple myeloma patients. Cancer Med. 2022; 00: 1- 11. doi: 10.1002/cam4.4770.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#多发性#
37
#新诊断#
53
#动脉高压#
37
#不良预后#
43
#预后因素#
40
#Med#
40