9月份病房遇到的病例
因突发左侧肢体无力,伴言语不利,外院行头部MRI示脑干急性脑梗病变,按“脑梗死”治疗2月余,患者仍不能发出声音,肢体活动不能抬离床面。
冒着糖尿病的风险给患者使用了激素治疗,皇天不负有心人,患者用药后第二天就发出了声音,无力的肢体可以抬离床面了。随着治疗及家属的积极配合,患者的病情一天天在好转,1个月的时间,患者可以讲话,尽管声音比较轻,并可以在家人搀扶下行走。
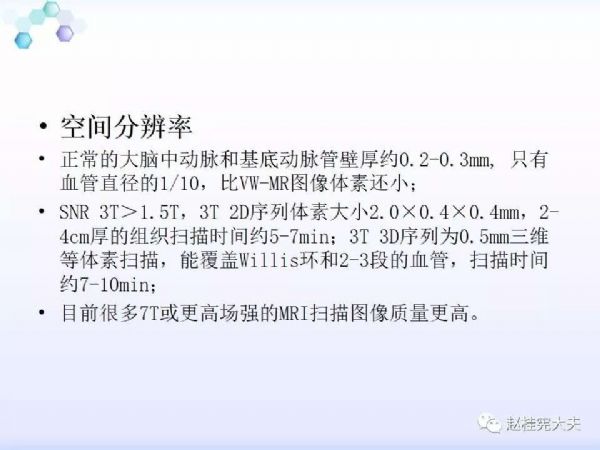
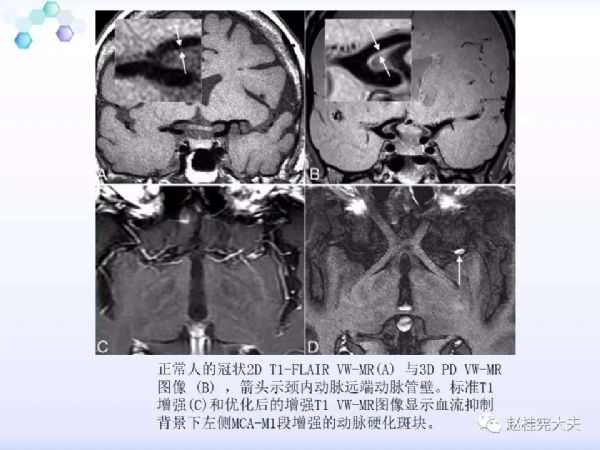
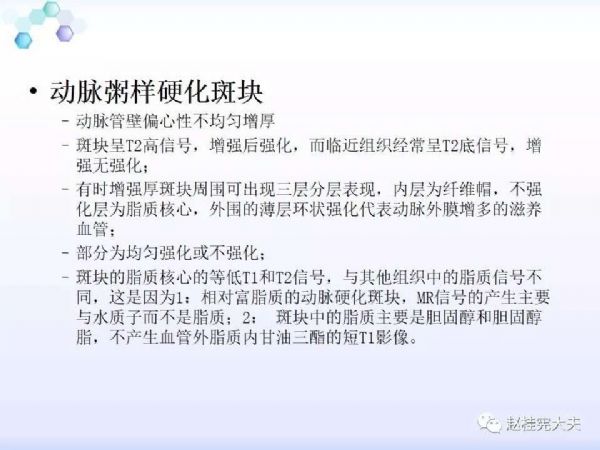
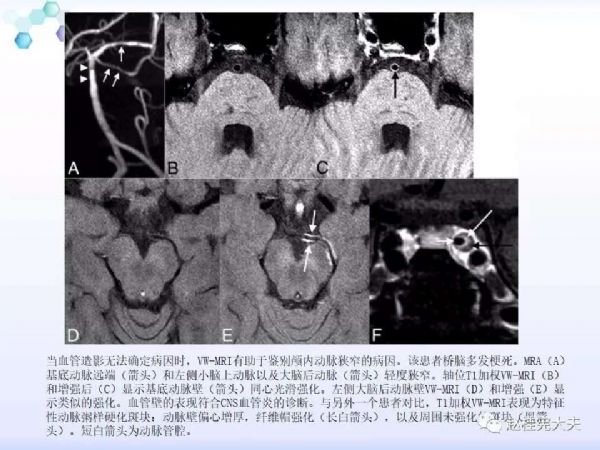
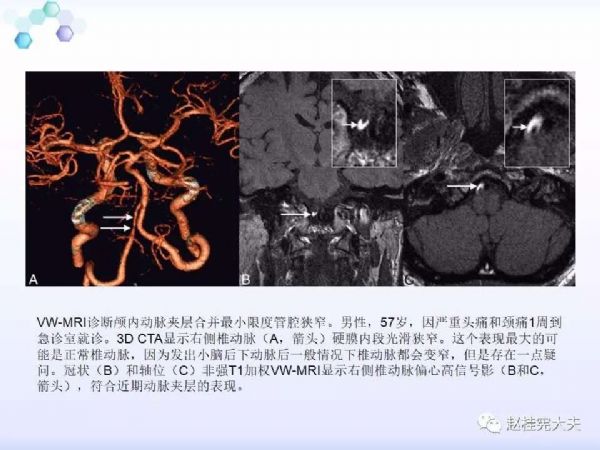
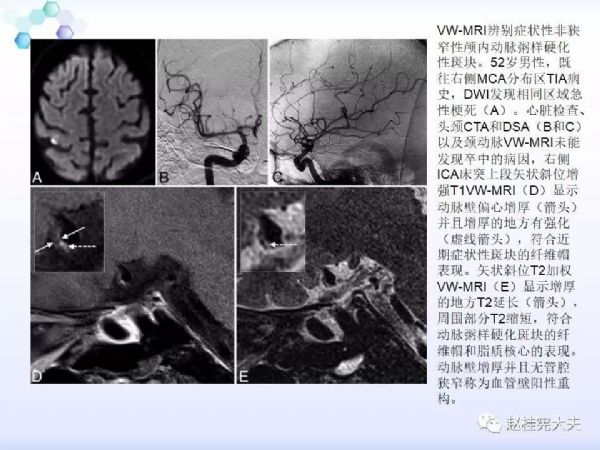
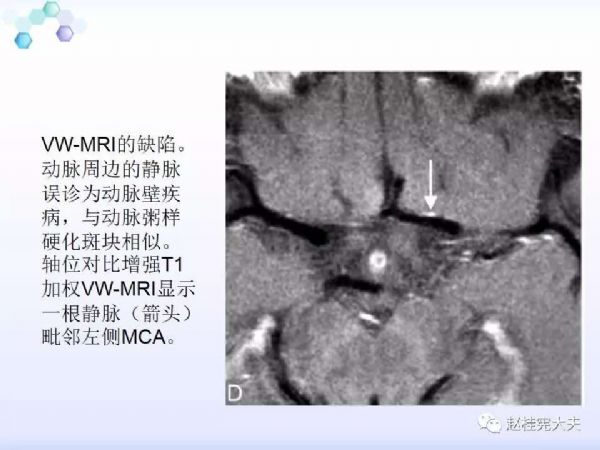
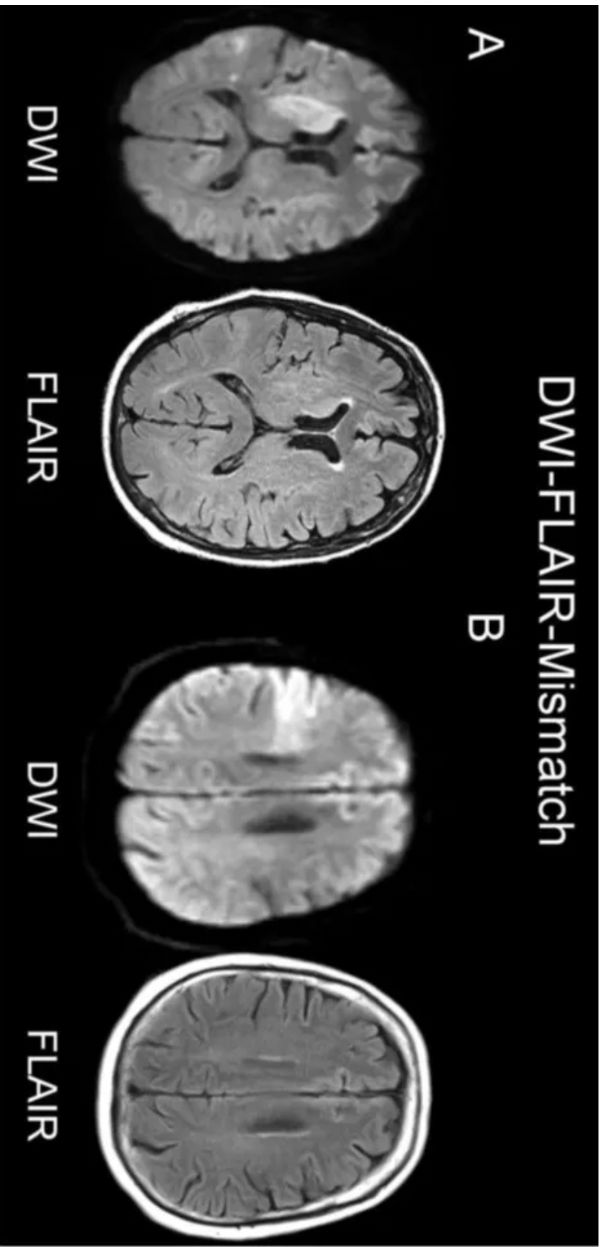
月份1个月长门诊遇到了好几例大脑中动脉或基底动脉狭窄致脑梗塞的患者,我特别关注了高分辨率血管壁MR成像技术在临床的应用。
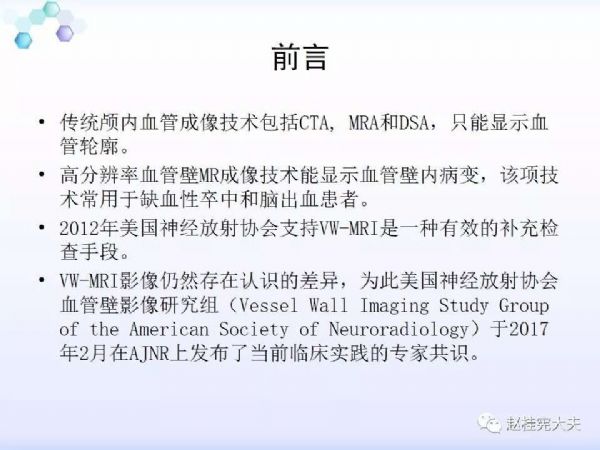
年初有篇文章(Intracranial Vessel Wall MRI: Principles and Expert ConsensusRecommendations of the American Society of Neuroradiology)详细讲解了这项技术在脑血管病(缺血性卒中和脑出血)中的应用,深圳宝安医院放射科的宋建勋主任和赵双全主任翻译了本文,经同意,将翻译后的内容发在公众号中做个科普,再此,向两位主任表示感谢!
■ 以下将分享文章中的内容:
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言




















#脑梗塞#
42
#脑梗#
30
锦绣香江休息休息奖学金小鸡鸡都惦记解答解答解答惊喜惊喜惊喜惊喜惊喜惊喜
76
婚纱
72
呵呵哈哈哈
1