心血管病是威胁我国居民生命和健康的重大公共卫生问题,每年导致死亡人数达 400 万,占总死亡的 40% 以上,也是伤残和寿命损失的重要原因。近年来,β 受体阻滞剂已广泛应用于心血管疾病的治疗,成为多种心血管疾病的一线用药和基础用药,包括冠心病、心力衰竭、快速性心律失常、高血压等疾病。然而,β 受体阻滞剂种类繁多,各药物之间有何区别?临床又该如何选用?
一、β 受体阻滞剂的分类
β 受体阻滞剂是一种能选择性地与β 肾上腺素受体结合,从而拮抗神经递质和儿茶酚胺对 β 受体的激动作用药物。肾上腺素受体多数分布在交感神经节后纤维所支配的效应器细胞膜上,其受体分为选择性β1受体阻滞剂、非选择性β1 受体阻滞剂和兼有α1受体阻滞作用的 β 受体阻滞剂。
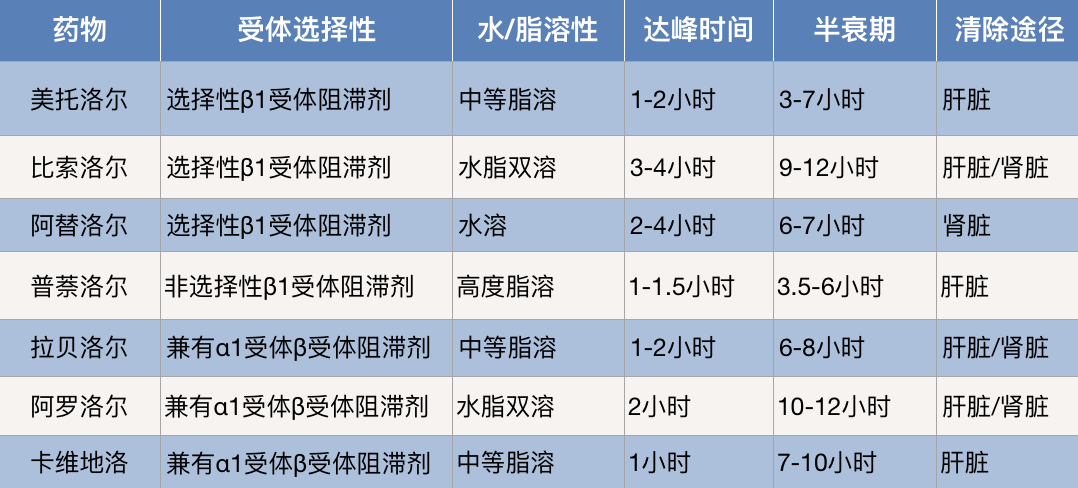
目前,临床上常用的β 受体阻滞剂包括美托洛尔、比索洛尔、阿替洛尔、普萘洛尔、拉贝洛尔、阿罗洛尔和卡维地洛等。其中,选择性β1受体阻滞剂有美托洛尔、比索洛尔和阿替洛尔等;非选择性β1受体阻滞剂为普萘洛尔;兼有α1受体阻滞作用的 β 受体阻滞剂包括括卡维地洛、阿罗洛尔和拉贝洛尔等。
β 受体阻滞剂药理和药代动力学特点
根据药代动力学特点,β 受体阻滞剂又分为脂溶性、水溶性和水脂双溶性。脂溶性β 受体阻滞剂是从胃肠道快速吸收, 在肠壁和肝内代谢,大部分经肝脏代谢,生物利用度低,可通过血脑屏障,而水溶性β 受体阻滞剂经胃肠道吸收不完全,多以原形或活性代谢产物从肾脏排出,很少通过血脑屏障。另外,水脂双溶性β 受体阻滞剂兼具溶/脂溶性B受体阻滞剂的特点。
二、β 受体阻滞剂的使用
1、美托洛尔应用于高血压、心绞痛、心肌梗死、肥厚型心肌病、主动脉夹层、心律失常、甲状腺机能亢进等。
用法用量:对于高血压的治疗,推荐100~200mg/次,一日2次,在血液动力学稳定后立即使用。 在治疗心绞痛、心律失常、肥厚型心肌病、甲状腺机能亢进等疾病时,一般25~50mg/次,一日2~3次,或100mg /次,一日2次。
另外,在急性心肌梗死、不稳定型心绞痛治疗中,应立即静脉给药一次 5 mg,在间隔 2分钟后重复给予,直到最大剂量 15 mg。之后15分钟开始口服25~50mg,每6~12小时一次,共24~48小时,然后口服50~100mg/次,一日2次。
值得注意的是,在药物相互作用中,美托洛尔与西咪替丁合用或预先使用奎尼丁均可增加美托洛尔的血浆浓度。另外,与利血平合用可增强美托洛尔的作用,需要注意低血压与心动过速。
2、比索洛尔主要用于高血压(可单独使用或与其他抗高血压药合用)、充血性心力衰竭。而对于比索洛尔过敏者、心源性休克、低血压、明显的心功能衰竭、Ⅱ或Ⅲ度房室传导阻滞、病态窦房结综合综合征、明显的窦性心动过缓和支气管哮喘者禁用。
用法用量:比索洛尔通常初始剂量为每次5mg,每天1次,对有支气管痉挛的患者初始剂量可为2.5mg。剂量可增加至10mg,如必要可加到20mg。另外,有肝、肾功能不全的患者(肌酐清除率小于每分钟40mL),使用初始剂量每天2.5mg,在剂量递增时要谨慎,因为比索洛尔不可以透析置换。
3、阿替洛尔常常用于高血压、心绞痛、心肌梗死、心律失常、甲状腺功能亢进等,也可用于嗜铬细胞瘤及青光眼等。
用法用量:成人常用口服剂量开始时,每次 6.25~12.5 mg,每日 2 次,按需要及耐受量逐渐增至 50~200 mg。肾损害时,肌酐清除率 < 15 mL/(min•1.73m²) 者,每日 25 mg;15~35 mL/(min•1.73m²) 者,每日最多 50 mg。
4、普萘洛尔主要用于治疗多种原因所致的心律失常,如房性及室性早搏、窦性及室上性心动过速、心房颤动等,但室性心动过速宜慎用。锑剂中毒引起的心律失常,当其他药物无效时,可试用普萘洛尔。此外,普萘洛尔也可用于心绞痛、高血压、嗜铬细胞瘤等。治心绞痛时,常与硝酸酯类合用。可提高疗效,并互相抵消其不良反应。
用法用量:高血压患者口服初始剂量10mg,每日3-4次,可单独使用或与利尿剂合用。剂量应逐渐增加,日最大剂量为200mg。心绞痛治疗,开始时5-10mg,每日3-4次;每3日可增加10-20mg,可渐增至每日200mg(20片),分次服。心律失常患者每次10-30mg,日服3-4次,应根据需要及耐受程度量。
另外,在治疗心肌梗死时,每日30-240mg,日服2-3次。肥厚性心肌病每日10-20mg,每日3-4次。按需要及耐受程度调整剂量。嗜铬细胞瘤患者10-20mg,每日3-4次。术前用三天,一般应先用α受体阻滞剂,待药效稳定后加用普萘洛尔。
5、拉贝洛尔主要用于心绞痛、轻至重度原发性高血压、妊娠高血压以及一些心律失常及麻醉过程中控制高血压。
用法用量:拉贝洛尔有100mg, 200mg和300mg三种口服药片。口服起始为每次100mg,每日2~3次。如疗效不佳,可增至每次200mg,每日3~4次。通常对轻、中、重度高血压的每日剂量分别为300~800mg、600~1200mg、1200~2400mg,加用利尿剂时可适当减量。
6、阿罗洛尔主要应用于轻度一中度原发性高血压、心绞痛、心动过速性心律失常和原发性震颤等。
用法用量:成人应用阿罗洛尔的口服剂量为每次10mg,每日2次。根据年龄、症状等适当增减剂量,疗效不充分时,可增至每日30mg。
7、卡维地洛主要应用于原发性高血压和有症状的充血性心力衰竭。
用法用量:推荐开始 2 周剂量为 3.125 mg/次,每日 2 次;若耐受性好,可间隔至少 2 周后将剂量增加 1 次,至 6.25 mg/次,每日 2 次,以此类推,增至每次 12.5 mg/次,每日 2 次;再至 25 mg/次,每日 2 次,剂量必须增加至患者能耐受的最高限度。体重 ≤ 85 kg,最大推荐剂量为 25 mg,每日 2 次;体重 > 85 kg,最大推荐剂量为 50 mg,每日 2 次。
三、β 受体阻滞剂不良反应
大剂量使用β 受体阻滞剂科可发生一些严重的不良反应。
1、心血管系统:可减慢心率,甚至造成严重心动过缓和房室传导阻滞,主要见于窦房结和房室结功能受损患者。
2、代谢系统:β 受体阻滞剂不影响胰岛素的降血糖作用,但Ⅰ型糖尿病患者应用非选择性 β 受体阻滞剂可掩盖低血糖的一些警觉症状,糖尿病患者或低血糖患者应慎用。
3、呼吸系统:可导致气道阻力增加,故禁用于哮喘或支气管痉挛性慢性阻塞性肺病,β2 受体存在于支气管平滑肌,β2受体兴奋时,支气管平滑肌松弛,当服用非选择性 β 受体 阻滞剂时,由于 β2 受体被阻断,使支气管收缩,增加呼吸道阻力,诱发或加重支气管哮喘的急性发作。
4、中枢神经系统: 可产生疲劳、头痛、睡眠紊乱、失眠、多梦和压抑等,特别是脂溶性高的 β 受体阻滞剂,易通过血脑屏障引起不良反应。
5、撤药综合征: 长期治疗后突然停药可发生高血压、心律失常、心绞痛恶化,其原因可能是交感活性的再现导致心肌需氧量突然增加、 血小板黏附力增加和反跳性高聚集、肾素-血管紧张 素活性增高、循环系统中甲状腺素和多巴胺水平增高 及 β 受体数目增多。
参考资料
1,刘健彤, 刘海燕. β受体阻滞剂在心血管疾病治疗中的应用[J]. 中国地方病防治杂志, 2017, 32(12):2.
2,樊小俊. β受体阻滞剂在治疗心血管疾病方面的应用现状研究[J]. 当代医药论丛, 2020, 18(7):2.
3,王先恒,赵长阔,黄梅,袁智,徐浪.美托洛尔的合成工艺研究[J].化学研究与应用,2018,30(05):846-850.
4,殷宇刚, 严斌. 比索洛尔干预高血压慢性心力衰竭左心室重构的研究[J]. 中华老年心脑血管病杂志, 2012, 14(10):3.
5,杨薇. 缬沙坦胶囊联合盐酸阿罗洛尔片对1~3期慢性肾脏病患者心肾功能的影响[J]. 中国实用医刊, 2017, 44(7):3.
6,姜红, 谢晋湘, 朱俊,等. 卡维地洛片剂Ⅰ期临床耐受性试验报告[J]. 中国医药导刊, 2002, 4(5):359-363.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#受体阻滞剂#
48
受益匪浅
42
学习了,很不错
61
#比索洛尔#
37
#阻滞剂#
39
#美托洛尔#
50
学习了,很好
64