2021 ACR:使用机器学习通过步态和身体活动预测2年内侧膝关节软骨恶化:MOST 研究
2021-11-25 MedSci原创 MedSci原创
该研究的目标是在多中心骨关节炎研究(MOST)中使用机器学习研究步态和身体活动预测2年的内侧胫股软骨恶化的能力。
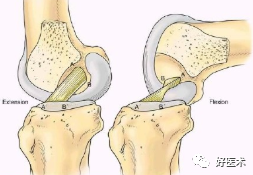
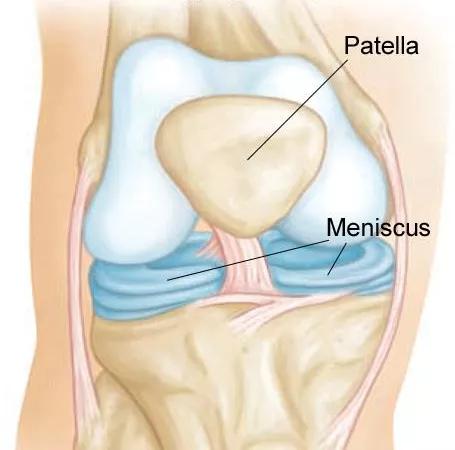
目的:识别有骨关节炎(OA)恶化风险的膝盖有助于识别需要干预的患者。虽然步态和体力活动对膝关节OA发病很重要,但这些因素之间的相互关系很复杂,使用传统统计模型来研究具有挑战性。机器学习方法无需在预测结果时预先指定这些因素之间的潜在关系。该研究的目标是在多中心骨关节炎研究(MOST)中使用机器学习研究步态和身体活动预测2年的内侧胫股软骨恶化的能力。
方法:从有和无膝关节疼痛或放射学OA参与者中收集人口统计学和临床数据、自选速度步行期间的地面反作用力(GRF)数据以及佩戴加速度计7天的身体活动数据。在基线和2年随访时,由两名肌肉骨骼放射科医生在5个胫股内侧亚区中使用MRI骨关节炎膝关节评分(MOAKS)评估膝盖软骨损伤。任何亚区域的软骨大小或深度MOAKS评分恶化定义为进展。排除Kellgren-Lawrence分级> 2的膝盖以关注早期疾病阶段。“超级学习”(一种集成机器学习方法)用于预测软骨恶化,来自标准化GRF、加速度计和人口统计/临床特征数据用超过100次随机方法分成70%训练数据和30%测试数据。使用AUC评估性能。重要预测因子定义为在100个数据拆分中最常出现在前10个预测贡献者中的10个特征(通过可变重要性度量统计)。边际效应图用于确定关联方向。
结果:分析包括了1323个参与者,14%内侧软骨在2年内恶化。在100次模型运行中,保留测试集的中位数AUC(第2.5和第97.5个百分位数)为0.78 (0.73-0.85)。重要预测因素(前10名的出现频率)包括:基线内侧软骨损伤(100)、Kellgren-Lawrence等级(83)、步行时间百分比(80)、坐/站时间百分比(65)、年龄(65)、 %时间躺着(62)、%其他活动时间(61)、活动水平(54)、内侧GRF冲动(37)和站立时间(31)。软骨恶化与较低的行走时间百分比、坐/站时间百分比和活动水平、较高的躺卧时间百分比和内侧GRF冲动以及较长的站立时间相关。
结论:结合步态、身体活动和临床/人口特征的集成机器学习方法在预测两年内软骨恶化方面表现出良好的性能。虽然确定模型中预测因子和软骨损失结果之间的关系并不简单,但该分析表明,解决步行时间短和整体活动水平低和/或内侧GRF冲动等问题可能是减少内侧胫股软骨恶化的潜在方法。
出处:
Costello K, Felson D, Jafarzadeh S, Segal N, Lewis C, Nevitt M, Lewis C, Kolachalama V, Kumar D. Using Machine Learning to Predict Medial Knee Cartilage Worsening over 2 Years Using Gait and Physical Activity: The MOST Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 10).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#关节软骨#
46
#步态#
35
#ACR#
45
#身体活动#
33
#机器#
35