EClinical Medicine:鱼油中的这种关键成分,才是改善心血管的关键?
2021-07-13 “心关注”公众号 “心关注”公众号
美国学者最新的荟萃分析,探究了ω-3脂肪酸对致死性/非致死性心血管结局的影响,以及EPA对比EPA+DHA 的治疗效果差异,结果已发表在了《EClinical Medicine》杂志上。
说到ω-3脂肪酸,人们对其在降低心血管事件发生风险上,关注度一直比较高。不少学者也陆续提出了ω-3脂肪酸可降低甘油三酯、抗血栓形成、抗炎或抗心律失常等可能的心血管保护机制。
不过,近几年多项国际大型研究的结论却并不一致,ω-3脂肪酸究竟有没有心血管保护作用?其中EPA、DHA成分作用大不大?
美国学者最新的荟萃分析,探究了ω-3脂肪酸对致死性/非致死性心血管结局的影响,以及EPA对比EPA+DHA 的治疗效果差异,结果已发表在了《EClinical Medicine》杂志上。
在合并分析了38项研究的149051例受试者后发现:
相比对照组,ω-3脂肪酸组人群,心血管死亡风险降低7%,非致命性心梗风险降低13%,冠心病事件风险降低9%,主要不良心血管事件风险降低5%,血运重建风险降低9%。
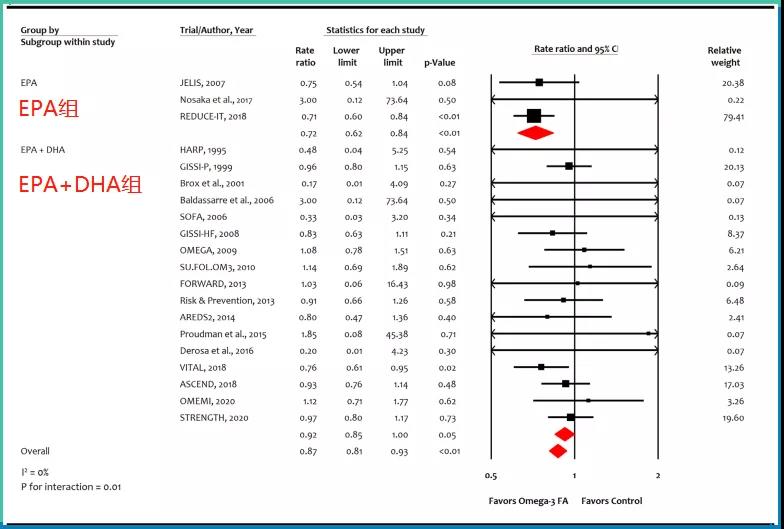
图片:ω-3脂肪酸对非致死性心肌梗死的影响
相比EPA+DHA,单用EPA的效果似乎更好。单用EPA组与EPA+DHA组在各结局事件风险降低程度上的对比,分别为:
心血管死亡:18% vs 6%;
非致死性心梗:28% vs 8%;
冠心病事件:27% vs 6%;
主要不良心血管事件和血运重建的风险降低,也是单用EPA更佳。这可能与EPA、DHA之间较大的结构与生理作用差异相关。
不过,ω-3脂肪酸组的房颤风险增加了26%,单用EPA组的房颤和出血风险也更高,分别增加了35%和49%。
这项研究肯定了ω-3脂肪酸在降低心血管死亡率、改善心血管预后方面的作用,并认为单用EPA的效果更佳。

所以,是时候多去买点鱼油类保健品了?笔者在这里并不推荐,市面上的很多保健品往往并不可靠,对于一般人群,还是建议多从鱼类食物中获取。
原始出处:
Safi U. KhanAhmad N. LoneMuhammad Shahzeb Khan, et al. Effect of omega-3 fatty acids on cardiovascular outcomes: A systematic review and meta-analysis. EClinicalMedicinePublished: July 8, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言





.jpg)






#CIN#
26
#DIC#
32
#clinical#
25
#Medicine#
33
#Med#
32
厉害👍
63