JAMA Intern Med:孕期服用抗精神病药物不会导致后代自闭症谱系障碍和注意力缺陷多动障碍风险增加
2022-05-23 MedSci原创 MedSci原创
孕期服用抗精神病药物不会导致新生儿自闭症谱系障碍和注意力缺陷多动障碍风险增加,略微增加早产以及出生低体重风险,鉴于怀孕期间抗精神病药物的收益,本研究不支持女性怀孕期间停止接受常规抗精神病药物治疗。

抗精神病药物,包括第一代和第二代抗精神病药物,近年来孕妇抗精神病药物使用率不断增加,然而孕期使用抗精神病药物的安全性尚未得到充分研究。有研究发现,孕妇使用抗抑郁药物可能导致新生儿神经发育障碍和出生并发症风险增加,包括自闭症谱系障碍(ASDS)、注意力缺陷多动障碍(ADHD)、早产和低体重等,但上述研究不能排除抗抑郁药自身不良事件以及遗传因素的影响。近日研究人员就产前抗精神病药物暴露与新生儿出生风险和神经发育异常之间的关系进行了考察。

本次以人群为基础的队列研究在香港开展,招募2001年1月至2015年1月期间出生的儿童,随访至2019年12月,排除妊娠期服用抗抑郁药物或锂剂的孕妇。通过收集孕妇妊娠期药物史和个体药物史以及进行兄弟姐妹匹配分析,避免混淆影响。研究的主要终点为早产(妊娠小于37周)、低体重(出生体重比胎龄平均水平低2个标准差)、儿童注意缺陷/多动障碍(ADHD)和自闭症谱系障碍(ASD)。
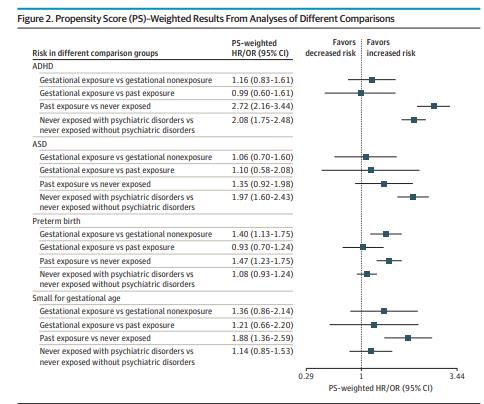
333749 对母婴参与ADHD风险分析(母亲分娩平均年龄31.46岁),411251 对母婴参与ASD、早产和低体重分析(母亲分娩平均年龄31.56岁)。有13196 名儿童(3.95%)被诊断为ADHD,8715名儿童(2.12%)患有ASD,33 891 名新生儿(8.24%)早产,7009名新生儿(1.70%)出生体重较低。与无抗精神病药物暴露人群相比,抗精神病药物暴露导致ADHD(HR=1.16)、ASD(1.06)风险略微增加,但导致早产(1.40)以及出生低体重风险显著增加(1.36)。对产妇的用药史进行分析后,孕期抗精神病药物暴露与ADHD(HR=0.99)、ASD(1.10)、早产(0.93)无关,略微增加出生低体重风险(1.21)风险。兄弟姐妹匹配分析后,孕期抗精神病药物暴露与ADHD(HR=0.41)、ASD(0.90)以及出生低体重风险(0.86)无关,略微增加早产风险(1.25)。
孕期抗精神病药物暴露与新生儿神经发育障碍和出生并发症
研究认为,孕期服用抗精神病药物不会导致新生儿自闭症谱系障碍和注意力缺陷多动障碍风险增加,略微增加早产以及出生低体重风险,鉴于怀孕期间抗精神病药物的收益,本研究不支持女性怀孕期间停止接受常规抗精神病药物治疗。
原始出处:
Zixuan Wang et al. Association Between Prenatal Exposure to Antipsychotics and Attention-Deficit/Hyperactivity Disorder, Autism Spectrum Disorder, Preterm Birth, and Small for Gestational Age. JAMA Intern Med. August 16,2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#注意力缺陷多动障碍#
39
#多动障碍#
35
学习了
0
#自闭症谱系障碍#
39
#抗精神病药#
33
#注意力#
33
#自闭#
35
#Med#
29
学习到了
60
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
38