JCO:低剂量他莫昔芬预防乳腺上皮内瘤变复发:随机安慰剂对照试验
2019-04-12 海北 MedSci原创
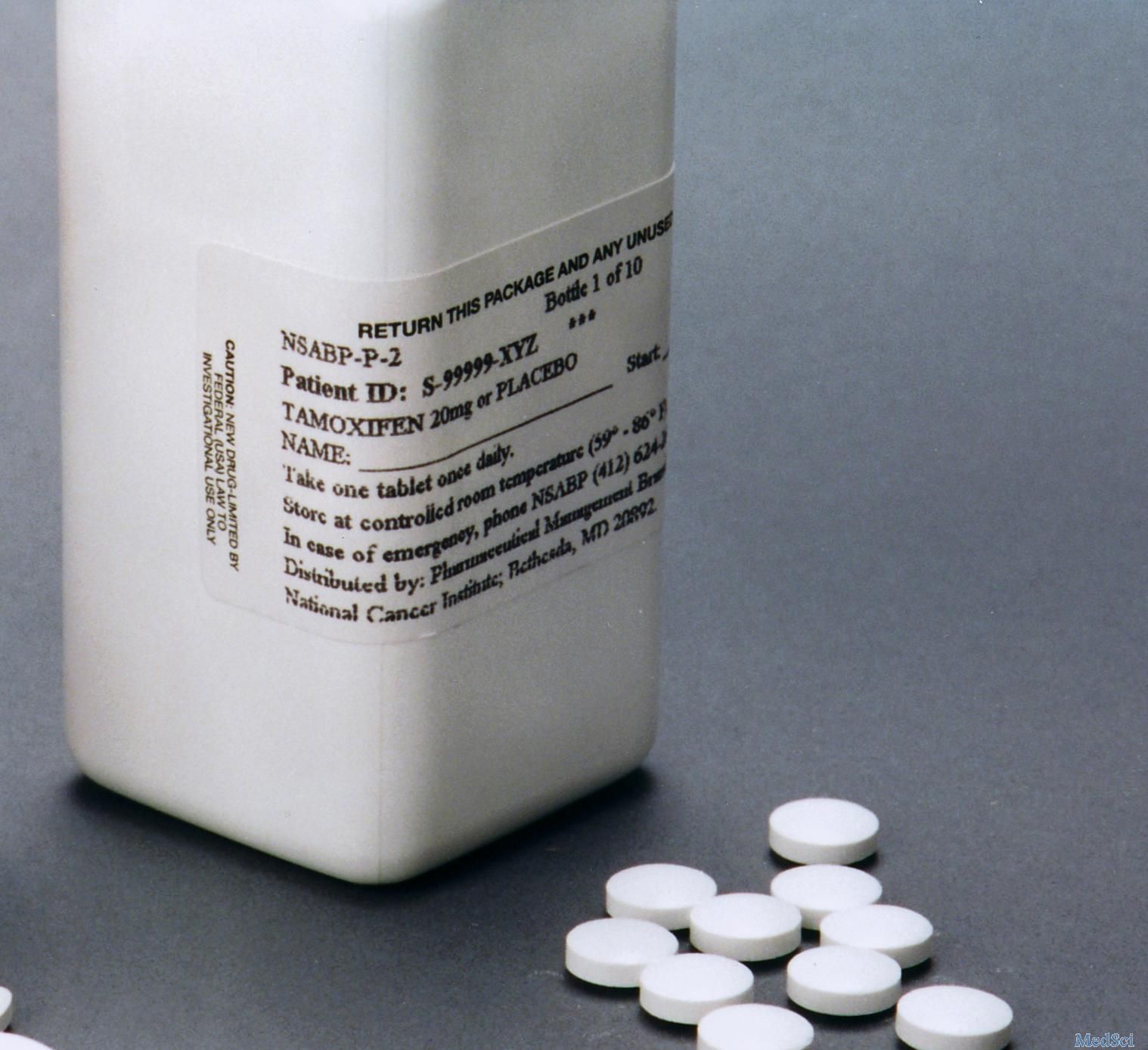
他莫昔芬以20 mg/d的剂量给药5年,对乳腺癌的治疗和预防有效,但毒性限制了其广泛使用。生物标志物试验显示,在减少乳腺癌增殖中,5mg / d的效果不低于20mg / d。
他莫昔芬以20 mg/d的剂量给药5年,对乳腺癌的治疗和预防有效,但毒性限制了其广泛使用。生物标志物试验显示,在减少乳腺癌增殖中,5mg / d的效果不低于20mg / d。
因此,研究人员提出假设,较短时间给予较低剂量可有效预防乳腺上皮内瘤变复发,但毒性低于标准剂量。
研究人员对患有激素敏感或未知乳腺上皮内瘤变的女性(包括非典型导管增生和原位小叶或导管癌)进行了一项多中心随机试验,其中包括他莫昔芬,5 mg / d,或安慰剂治疗3年。主要终点是浸润性乳腺癌或原位导管癌的发病率。
该研究包括了500名75岁或以下的女性。中位随访5.1年(四分位数间距3.9-6.3年)后,他莫昔芬治疗组有14例肿瘤事件,而安慰剂组有28例(11.6 v 23.9 / 1000人年;危险比,0.48;;95%CI,0.26至0.92;P = .02)。
他莫昔芬使对侧乳房事件减少75%(3个vs 12个事件;风险比,0.25; 95%CI,0.07至0.88;P = .02)。
除了使用他莫昔芬的每日潮热频率略有增加外,患者报告的结果在两组之间没有差异(P = .02)。他莫昔芬有12例严重不良事件,安慰剂组有16例,其中他莫昔芬组的1例为深静脉血栓形成,1例为子宫内膜癌,安慰剂组为1例肺栓塞。
因此,使用5mg / d的他莫昔芬3年可以在有限的毒性范围内,使乳腺上皮内瘤变复发减半,这为这些疾病提供了新的治疗选择。
原始出处:
DeCensi A et al. Randomized Placebo Controlled Trial of Low-Dose Tamoxifen to Prevent Local and Contralateral Recurrence in Breast Intraepithelial Neoplasia. JCO, 2019; doi: 10.1200/JCO.18.01779.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#JCO#
26
#对照#
32
#对照试验#
32
#安慰剂#
39
#他莫昔芬#
40
#低剂量#
34
#安慰剂对照#
37