Neurology CP:肝硬化相关血管病的发病机制
2018-07-16 杨中华 脑血管病及重症文献导读
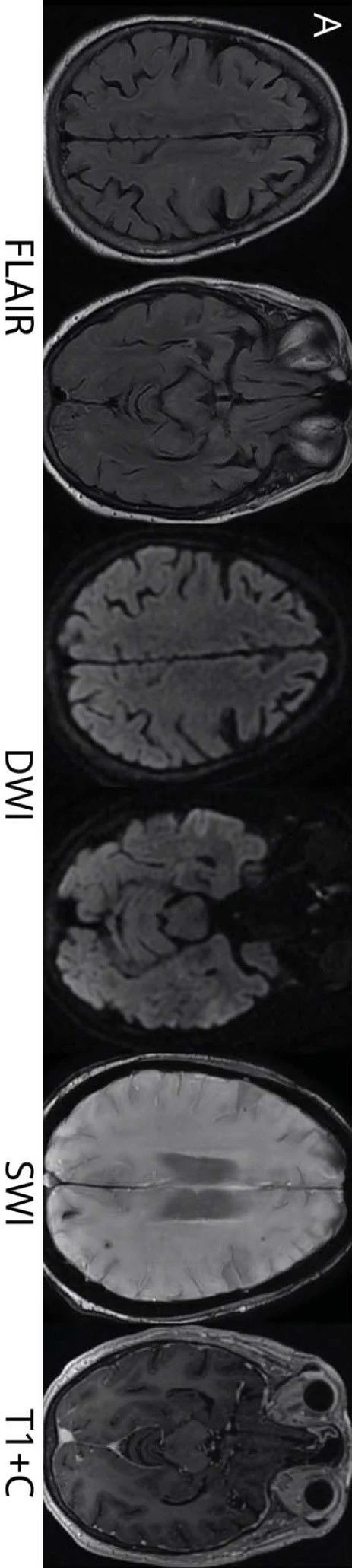
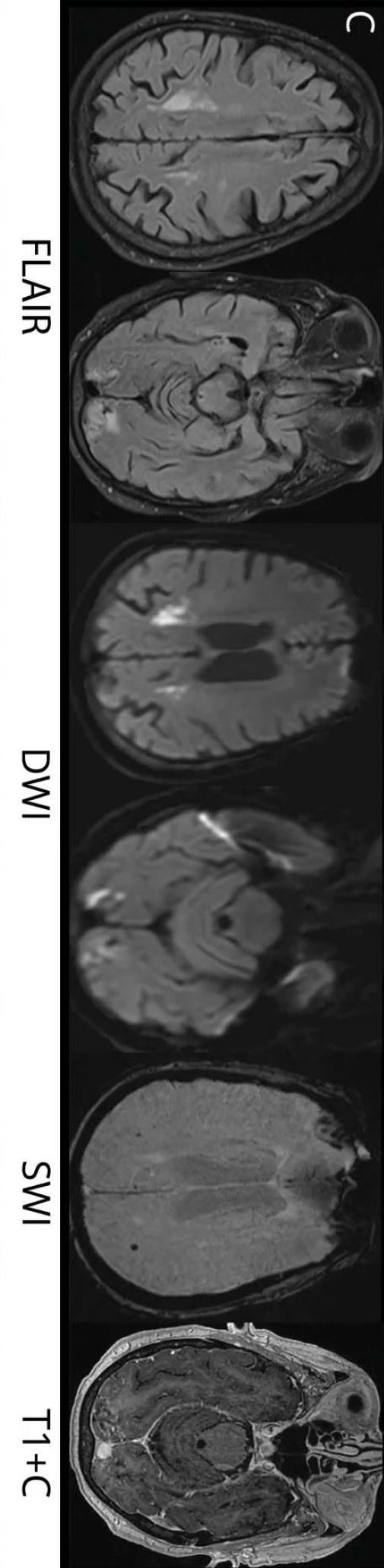
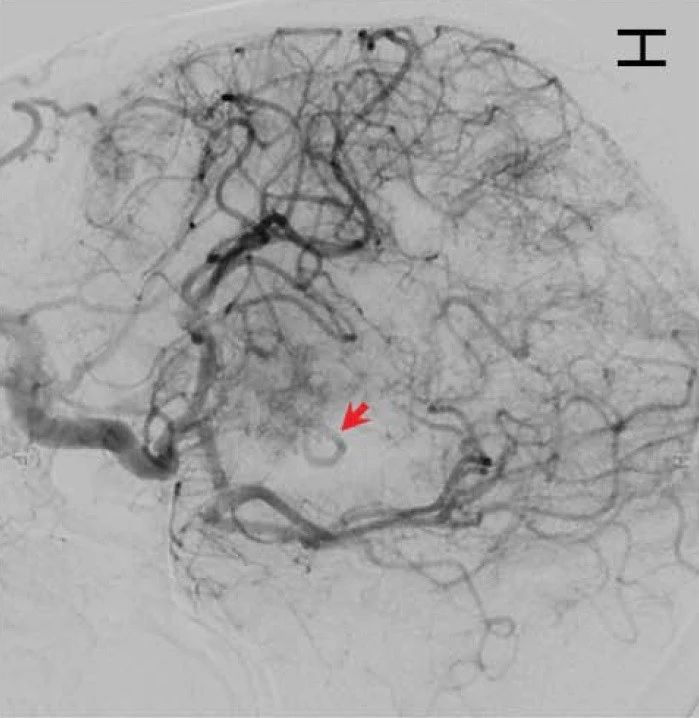
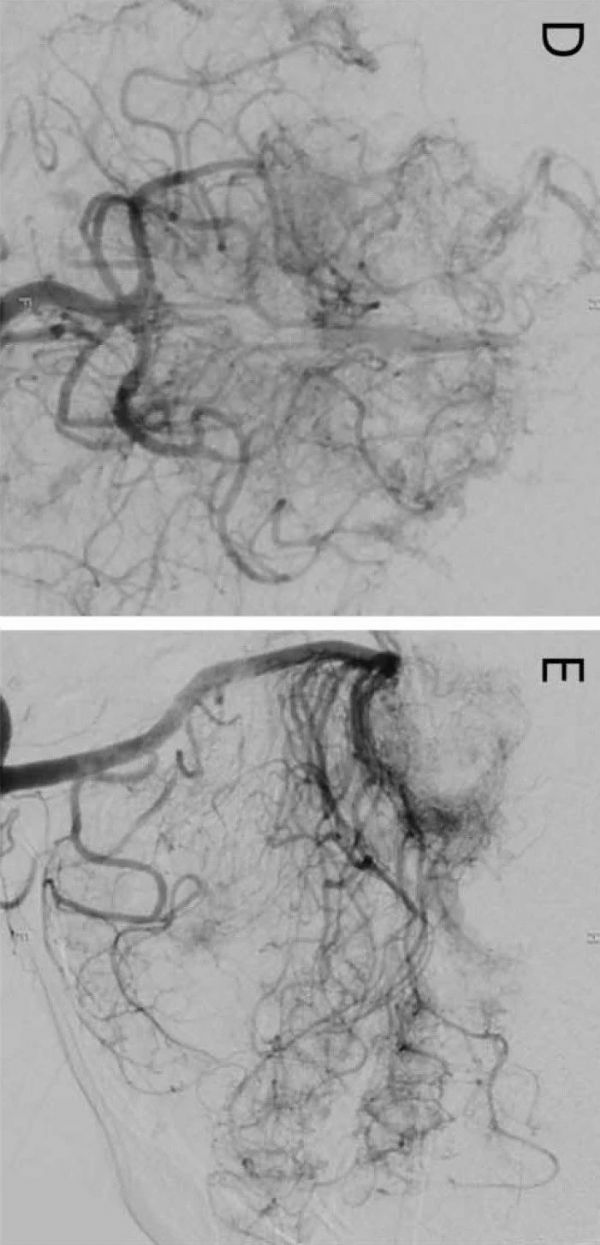
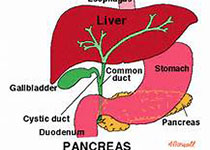
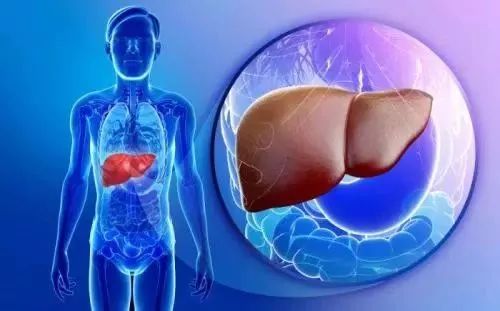
肝硬化对脑血管病的影响是多方面的,比如增加脑出血的风险,同时降低缺血性卒中的风险。尽管有报道显示颅内出血和血管畸形与肝脏疾病有关,其病理生理机制尚不清楚。肝硬化会引起于肝肺综合征(hepatopulmonary syndrome,HPS),后者表现为远端肺动脉扩张、扭曲,产生分流,甚至发生动静脉(arteriovenous,AV)畸形。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#血管病#
49
#Neurol#
49
谢谢分享学习
95
谢谢!最新的信息读起来就是收获大
58
学习了.不错的.谢谢分享.
74
谢谢分享学习
71