Alzheimer's & Dementia:老年人晚年的体力活动与脑组织突触完整性标记有关
2022-01-23 影像小生 MedSci原创
该研究第一次证明了生活方式行为、PA和人类脑组织突触完整性标记之间的联系
身体活动(PA)被广泛推荐用于与年龄相关的大脑健康的研究,但它的神经生物学还不是很清楚。动物模型表明PA具有突触性。
Kaitlin Casaletto等在Alzheimer's & Dementia杂志发表文章,研究了PA和老年人突触完整性标志物之间的关系。
来自Rush记忆和衰老项目的受试对象完成了年度活动监测(平均访视次数= 3.5±2.4)和死后评估。对脑组织突触前蛋白(突触素、突触totagmin-1、囊泡相关膜蛋白、合成蛋白、复合物I和复合物II)和神经病理学进行分析。模型检测了老年PA(平均每次访问)和时间特异性PA(尸检时间)与突触蛋白之间的关系。

晚年平均体力活动的增加与死亡时脑组织中较高的突触蛋白相关,复合物- II除外。
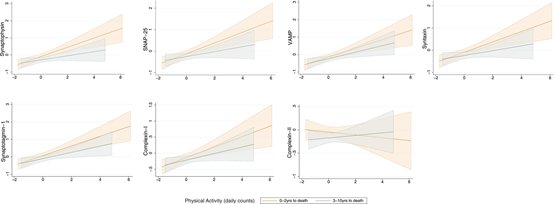
在时间上采取的措施越接近(即活动监测到死亡之间的时间),身体活动和脑组织突触蛋白水平之间的关系就越强。
更大的晚年PA与更高的突触前蛋白水平相关(0.14 <β<0.20),复合物-II除外(β = 0.08)。相关关系独立于病理,具有时间特异性;在2年内完成脑组织测量的参与者显示出最大的PA-突触蛋白关联(0.32<β<0.38)。PA和突触前蛋白之间的关系在脑区取样具有可比性。
该研究第一次证明了生活方式行为、PA和人类脑组织突触完整性标记之间的联系。PA可能有助于建立突触健康,即使是在晚期(如大脑储备),这种关联独立于病理,是一个潜在的可塑性过程,可能需要持续一段时间。
原文出处
Late-life physical activity relates to brain tissue synaptic integrity markers in older adults
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#dementia#
27
#完整性#
37
#突触#
53
#脑组织#
32