新版肺血栓栓塞症防治指南发布:D二聚体阴性,可基本除外急性肺栓塞
2018-04-11 岱西 中国循环杂志
近日,《肺血栓栓塞症诊治与预防指南》更新。该指南在2001年指南基础上,系统评价当前包括国人在内的循证医学资料,并对临床医生关注的临床问题和结局指标进行了凝炼。
新指南主要“新”在八个方面:
具体要点见下:
疑诊时推荐:推荐使用可能性评分
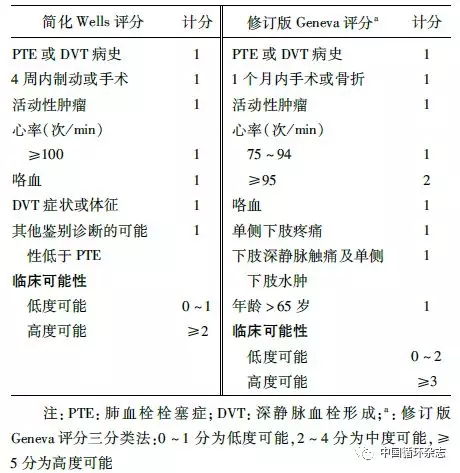
(1)推荐基于临床经验或应用临床可能性评分(简化的Wells评分、修订的Geneva评分量表)对急性PTE进行疑诊的临床评估(1 A)。
表1 PTE临床可能性评分表
(2)推荐临床评估联合D-二聚体检测进一步筛查急性PTE(1A)。
(3)临床评估低度可能的患者,如D-二聚体检测阴性,可基本除外急性PTE,如D-二聚体检测阳性,建议行确诊检查(1 A)。
(4)临床评估高度可能的患者,建议直接行确诊检查(1 A)。
确诊时推荐:建议完善CT肺动脉造影
(1)疑诊PTE患者,根据是否合并血流动力学障碍采取不同诊断策略(1C)。
(2)血流动力学不稳定疑诊患者:如条件允许,建议完善CT肺动脉造影(CTPA)检查以明确诊断或排除PTE;
如无条件或不适合行CTPA检查,建议行床旁超声心动图检查,如发现右心室负荷增加和(或)发现肺动脉或右心腔内血栓证据,在排除其他疾病可能性后,建议按PTE治疗;
建议行肢体加压静脉超声,如发现DVT的证据,则VTE诊断成立,并可启动治疗;在临床情况稳定后行相关检查明确诊断(2C)。
(3)血流动力学稳定疑诊患者:推荐将CTPA作为首选的确诊检查手段(1B);
如果存在CTPA检查相对禁忌(如造影剂过敏、肾功能不全、妊娠等),建议选择其他影像学确诊检查,包括核素肺通气/灌注(V/Q)显像、磁共振肺动脉造影(2B)。
求因:年龄相对较轻者,建议行易栓症筛查
(1)急性PTE患者,推荐积极寻找相关的危险因素,尤其是某些可逆的危险因素(如手术、创伤、骨折、急性内科疾病等)。
(2)不存在可逆诱因的患者,注意探寻潜在疾病,如恶性肿瘤、抗磷脂综合征、炎性肠病、肾病综合征等。
(3)年龄相对较轻(如年龄<50岁)且无可逆诱发因素的急性PTE患者,建议行易栓症筛查。
(4)家族性VTE,且没有确切可逆诱发因素的急性PTE患者,建议进行易栓症筛查。
危险分层:血流动力学不稳定者定义为高危
(1)建议对确诊的急性PTE患者进行危险分层以指导治疗。首先根据血流动力学状态区分其危险程度,血流动力学不稳定者定义为高危,血流动力学稳定者定义为非高危(2 C)。
(2)血流动力学稳定的急性PTE,建议根据是否存在右心功能不全(RVD)和(或)心脏生物学标志物升高将其区分为高危和低危(2 B)。
治疗推荐意见
一般支持治疗:急性PTE,若血流动力学稳定,在充分抗凝基础上,建议尽早下床活动(2C)
抗凝治疗:
临床高度可疑急性PTE,在等待诊断结果过程中,建议开始应用胃肠外抗凝治疗(UFH、LMWH、磺达肝葵钠)。(2C)
一旦确诊急性PTE,若无抗凝禁忌,尽早抗凝。(1C)
急性PTE,初始抗凝推荐选用LMWH、UFH、磺达肝葵钠、负荷量的利伐沙班或阿哌沙班(2B)。
急性PTE,若用华法林长期抗凝,推荐在应用胃肠外抗凝药物24 h内重叠华法林,调节INR为2.0~3.0,达标后停用胃肠外抗凝(1B)。不推荐常规药物基因组检测指导华法林剂量调节。
急性PTE,若选用利伐沙班或阿哌沙班,在使用初期需予以负荷剂量;若选择达比加群或依度沙班,应先给与胃肠外抗凝药物至少5 d(1B)。
抗凝疗程:
有明确可逆危险因素的急性PTE,在3个月抗凝治疗后,如危险因素去除,停用抗凝治疗(2B);
有危险因素持续存在的PTE,在3个月抗凝治疗后,建议继续抗凝治疗(2C);
特发性PTE治疗3个月后,若仍未发现确切危险因素,同时出血风险较低,推荐延长抗凝治疗时间,甚至终生抗凝(1C);
特发性PTE治疗3个月后,若出血风险高,根据临床情况,动态评估血栓复发与出血风险,以决定是否继续抗凝(2B)。
说明:延展期抗凝药物与初始药物一致,也可根据实际情况调整。若在延展期患者拒绝抗凝治疗或无法耐受抗凝药物,尤其是有冠心病史且因此服用抗血小板治疗者,可考虑给予阿司匹林口服进行VTE二级预防。
偶然发现或亚段PTE处理:
无症状偶尔发现的PTE,若存在VTE进展危险因素或复发风险,建议给予至少3个月抗凝治疗,推荐应用与急性PTE相同的方案(2C);
亚段PTE,若存在相关临床症状,建议给予至少3个月抗凝治疗,推荐应用与急性PTE相同的方案(2C);
亚段PTE(无症状且无下肢近端DVT),若VTE复发风险低,建议临床观察;若复发风险高,建议给予至少3个月抗凝治疗,推荐应用与急性PTE相同的方案(2C)。
复发性PTE或DVT抗凝治疗:
抗凝治疗期间,出现VTE复发,建议首先积极寻找复发原因(2C);
使用口服抗凝药物治疗过程中,出现VTE复发,建议暂时转换为LMWH治疗(2C);
接受长期LMWH抗凝治疗过程中,出现VTE复发,建议增加LMWH的剂量(2C)。
急性PTE溶栓治疗推荐意见:
急性高危PTE,若无溶栓禁忌则行溶栓治疗(1B),如溶栓治疗前需初始抗凝治疗,选择UFC(2C);非高危者,不推荐常规溶栓治疗(1C);
急性中高危PTE,建议先给予抗凝治疗,并密切观察病情变化,若临床恶化,且无溶栓禁忌,建议给予溶栓治疗(2B);
急性PTE应用溶栓药物,建议rt-PA 50 mg、尿激酶2万 U/kg或重组链激酶150万 U,2 h持续静脉滴注(2B);
急性PTE介入治疗和手术治疗:
急性高危PTE或伴临床恶化的中危PTE,若有肺动脉主干或主要分支血栓,并存在高出血风险或溶栓禁忌,或经溶栓或积极内科治疗无效,可行介入治疗(2C);
低危PTE不建议导管介入治疗(2C);
已接受抗凝治疗的急性DVT或PTE,不推荐放置下腔静脉滤器(1B)。
急性高危PTE,若有肺动脉主干或主要分支血栓,如存在溶栓禁忌、溶栓治疗或介入治疗失败、其他内科治疗无效,可考虑行肺动脉血栓切除术(2C)。
妊娠合并PTE的处理和诊断:
疑诊急性PTE:建议D-二聚体检测,若阴性可基本排除PTE(2C);建议行下肢CUS检查,一旦确诊DVT,即可按照VTE进行处理(2C);如下肢CUS检查阴性,临床仍高度怀疑PTE,建议行V/Q显像(2C);
合并急性PTE治疗:抗凝药物首选LMWH(1B),产后建议切换华法林(2B);溶栓仅限于危及生命的高危PTE(2C)。
恶性肿瘤合并PTE:
疑诊急性PTE,D-二聚体阴性具有除外诊断价值(2B);活动期恶性肿瘤合并VTE,建议给予LMWH抗凝治疗至少3~6个月(2B),若在抗凝治疗3个月后,出血风险不高,推荐抗凝时间延长,甚至终生抗凝(1C);
PTE合并活动性出血:
若为小出血,抗栓治疗同时积极对局部处理(2C);若大出血或临床相关非大出血,建议暂停抗凝治疗,并积极寻找出血原因并治疗(2C)。
围手术期PTE:
并发高危PTE:若发生于手术1周内,不建议溶栓治疗,必要时考虑介入治疗(2C);若在手术1周后,出血风险低可考虑溶栓治疗(2C);
对于正在行抗凝治疗的PTE患者如需手术:
使用华法林且存在VTE复发高风险,无大出血风险,建议术前5天停华法林并进行桥接抗凝(2C);
若接受胃肠外抗凝或桥接抗凝治疗,使用UFH者建议术前4~6 h停用,使用LMWH者,建议术前约24 h停用,术后24 h 重新启用,高风险手术,术后48~72 h 重新启用(2C);
如使用DOAC抗凝,需在术前暂时中断治疗,不建议进行桥接治疗(2C),建议根据肾功能、药物半衰期、出血风险停用及重新启用DOAC(2B)。
PTE合并右心血栓的处理推荐:
建议首选超声心动图进行诊断并评估右心血栓风险,同时鉴别非血栓性疾病(2C);
右心血栓,建议抗凝治疗至少3个月,并定期复查心脏超声,评估血栓变化和疾病风险(2C);
体积较大的右心新鲜血栓,建议UFH抗凝治疗,如出现血流动力学不稳定,严密监测下,建议行溶栓(2C);
有技术条件,建议外科取栓治疗适用于:体积较大的A型血栓;体积较大的C型血栓,并具有潜在堵塞右心房或右心室流出道的风险;骑跨于卵圆孔的右心血栓等(2C);
血小板减少合并PTE的处理推荐:
建议积极筛查血小板减少病因(2C);
若有肝素接触史,可使用4T评分来评估HIT可能性。若中高度临床可能性,推荐检测HIT抗体,HIT混合抗体或IgG特异性抗体阴性,可除外HIT(1B);IgG特异性抗体阳性可确诊HIT(1C);
若诊断HIT,建议停用UFH或LMWH(1A),更换为阿加曲班或比伐卢定(1B);早期不推荐应用华法林行初始治疗,当血小板恢复至150X109个/L时,可启用小剂量华法林。胃肠外非肝素抗凝药与华法林重叠至少 5 d,直至达到目标INR(1C);
HIT不伴血栓形成,建议抗凝治疗至少4周;伴血栓形成,抗凝治疗至少3个月(2B);
慢性血栓栓塞性肺动脉高压(CTEPH)治疗的推荐:
疑诊CTEPH:首选肺V/Q显像筛查,阴性可基本除外(1B);V/Q显像阳性,建议进一步行CTPA(1C)、右心导管和肺动脉造影(1B);
确诊CTEPH:若无禁忌,终生抗凝(1B);推荐手术评估,如能手术,首选PEA(1C);无法行PEA手术或术后存在残余肺动脉高压,建议应用靶向药物治疗(2B)或介入治疗(2C);
外科手术患者VTE预防推荐:
外科手术患者,建议应用Caprini评分,进行VTE风险分级(1B);推荐术后早期活动(2C);如不存在高出血分析,VTE风险低者,建议应用机械预防(2C),中度风险建议应用药物预防或机械预防(2B),高度风险,推荐应用药物预防(1B)或药物联合机械预防(2C)。
在线使用:Caprini血栓风险因素评估表
具有VTE风险者,若同时存在较高大出血风险或出血并发症:推荐应用机械预防,如出血风险降低,改用药物预防与机械预防联用(1B);
多数VTE高风险患者,建议药物或机械预防至术后7~4天(2C);对于合并恶性肿瘤的外科手术和骨科大手术,建议延长预防时间(2B);
外科手术患者,不建议应用下腔静脉滤器作为VTE的一级预防(2C);
出血可致严重后果的手术,建议应用机械预防(2C);当VTE风险为高度,如出血风险降低,建议改为药物预防联合机械预防(2C);
内科住院患者VTE的预防推荐:
建议应用Padua评分进行VTE分级(1B);推荐早期活动(2C);VTE高风险者,若不存在出血风险,推荐应用药物预防(1A),高出血风险,应用机械预防(1A);
活动期恶性肿瘤患者,如无其他VTE风险,单纯接受化疗不推荐常规预防(1C);留置中心静脉导管,不推荐常规预防(1B);
多数VTE高风险患者,建议药物或机械预防7~14 天(2C)。
原始出处:
中华医学会呼吸病学分会肺栓塞与肺血管病学组,中国医师协会呼吸医师分会肺栓塞与肺血管病工作委员会, 全国肺栓塞与肺血管病防治协作组. 肺血栓栓塞症诊治与预防指南. 中华医学杂志, 2018, 98(10): 1060-1087.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








学习了
46
#二聚体#
40
#肺血栓栓塞症#
35
#肺血栓#
37
#栓塞症#
43
#防治指南#
21
#急性肺栓塞#
41
学习了
56