NEJM:荧光素导向在胶质母细胞瘤切除术中的应用-案例报道
2017-05-04 xing.T MedSci原创
该患者术后四周,开始接受放疗和替莫唑胺治疗。术后2个月随访,该患者无头痛症状,以及无神经功能缺损。
患者为一名55岁的男性,因剧烈头痛1周而于急诊就诊。有和无钆为基础的造影剂的大脑磁共振成像显示在右颞叶大脑边缘增强肿块(直径为4.5厘米)。
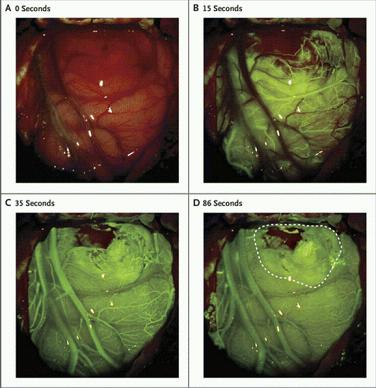
在肿瘤切除手术时,给予静脉注射荧光素,A组显示在注射前的基础情况。正常脑实质其完整的血脑屏障可以防止荧光素的吸收;然而,肿瘤可破坏血脑屏障,允许荧光团的积累。在这个病人中,在注射荧光素后的第一个35秒内,荧光首先出现在动脉血管(如图B所示),然后出现在较小的静脉,然后再出现在较大的静脉(如图C所示)。注射后35秒,荧光素开始积聚在肿瘤组织中(如图C所示)。在注射后86秒时,皮质静脉内的荧光素开始褪色,肿瘤(如图D所示,虚线内的区域)和周围的正常组织之间形成了鲜明的对比;一小部分血液掩盖了一些肿瘤组织。
该患者术后四周,开始接受放疗和替莫唑胺治疗。术后2个月随访,该患者无头痛症状,以及无神经功能缺损。
原始出处:
David W. Roberts,et al. Fluorescein Guidance in Glioblastoma Resection.N Engl J Med 2017; http://www.nejm.org/doi/full/10.1056/NEJMicm1611258
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#母细胞瘤#
33
#胶质母细胞#
32
#荧光#
33
#切除术#
32
#细胞瘤#
36
学习,感谢分享!
75