Int J Biol Sci:Livin与Ras的协同作用诱导并维持气道粘膜的皮质类固醇抗性
2021-07-09 AlexYang MedSci原创
有许多疾病,如慢性肺部疾病、慢性肾脏疾病、炎症性肠病、类风湿性关节炎等,都依赖于对非特异性抑制炎症有强烈作用的类固醇治疗。为了控制症状,类固醇治疗通常需要很长的时间,有些病人甚至需要终生使用。在这些病
有许多疾病,如慢性肺部疾病、慢性肾脏疾病、炎症性肠病、类风湿性关节炎等,都依赖于对非特异性抑制炎症有强烈作用的类固醇治疗。为了控制症状,类固醇治疗通常需要很长的时间,有些病人甚至需要终生使用。在这些病人中,多达30%的人对中等剂量的皮质类固醇没有反应,这种情况称为皮质类固醇抵抗(CR)。

皮质类固醇抵抗(CR)严重影响了类固醇对许多慢性炎症的治疗效果,包括气道过敏。CR的产生机制尚不清楚。近期的研究表明,一种凋亡抑制剂-livin,与细胞活动的调控有关。最近,有研究人员探讨了livin在诱导和维持气道粘膜CR中的作用。
研究人员从手术切除的过敏性鼻炎(AR)和鼻息肉患者的鼻粘膜组织中分离出鼻上皮细胞(NECs),他们患有或者不患有CR。通过RNA测序分析了NECs中的差异表达基因,并建立了一个CR小鼠模型,以测试livin在CR发展中的作用。
结果显示,患有CR的AR患者的NECs表达了高水平的livin,这与NECs中胸腺基质淋巴细胞生成素(TSLP)的表达和Ras的高度激活状态呈正相关。在诱导和维持NECs中TSLP的表达方面,Livin和Ras激活具有相互促进作用。TSLP能够诱导嗜酸性粒细胞和中性粒细胞表达糖皮质激素受体-β(GRβ)。CRβ高表达的嗜酸性粒细胞和中性粒细胞对皮质类固醇具有抗性。消除livin或抑制TSLP可明显减弱CR和气道过敏。
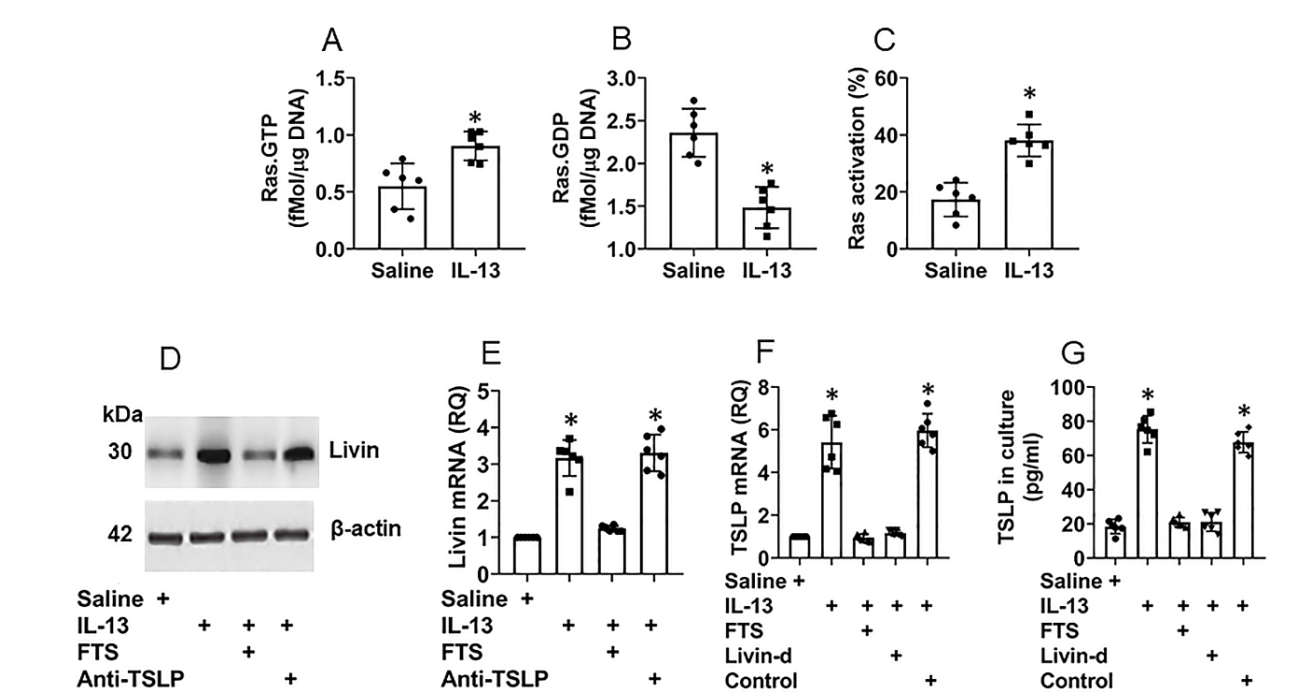
Ras激活和livin与NECs中TSLP的表达有关
综上所述,Livin通过促进上皮细胞中TSLP的表达和嗜酸性粒细胞和中性粒细胞中GRβ的表达促进了气道中CR的发展。消除Livin或抑制TSLP可减弱CR的发展并抑制气道过敏,该结果有转化的潜力,可用于治疗气道过敏。
原始出处:
Jin-Mei Xue , Yun-Fang An , Li-Min Suo et al. Livin in synergy with Ras induces and sustains corticosteroid resistance in the airway mucosa. Int J Biol Sci. 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Bio#
35
#粘膜#
48
#Biol#
28
#抗性#
31
#类固醇#
42