Nat Cell Biol:“饿死”胰腺癌——双管齐下,“癌王”能否束手就擒?
2019-11-22 Ruthy 转化医学网
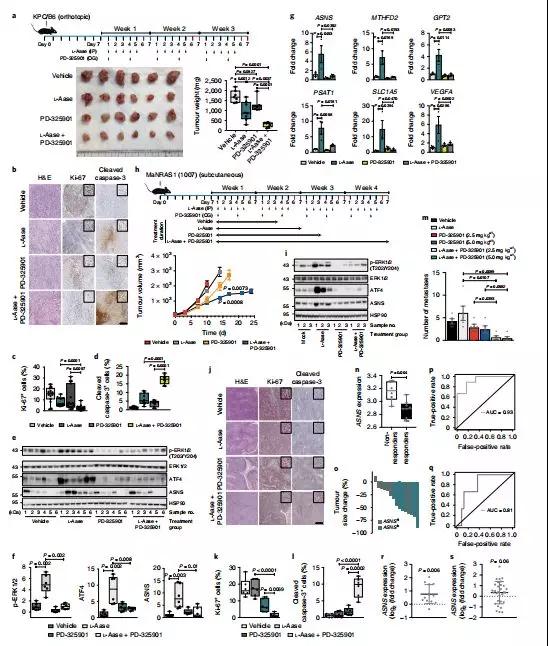
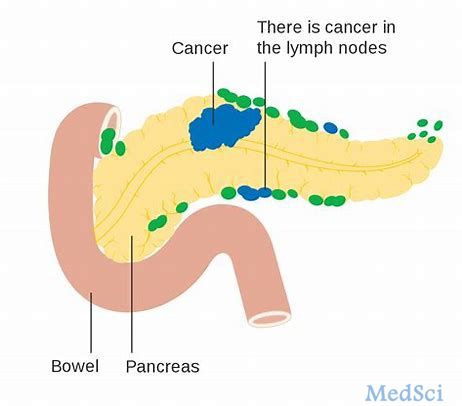
胰腺癌是一种恶性程度很高的消化道胰腺癌,诊断和治疗均极为困难,5年生存率<1%,是预后最差的恶性胰腺癌之一。快速增殖的胰腺癌细胞需要生物大分子提供能量和生物合成基础,因此细胞营养限制成为了治疗胰腺癌的潜在策略,其中利用L-天冬酰胺酶抑制天冬酰胺的疗法受到广泛关注。但是该方法在胰腺癌治疗中的应用效果与预期相去甚远,而解决方案尚未有定论。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Bio#
34
#Cell#
32
#CEL#
31
#Biol#
19
#Nat#
19