J Bone Miner Metab:洛索洛芬可抑制唑来膦酸诱导的急性期反应
2020-12-09 网络 网络
唑来膦酸输液用于治疗骨质疏松症,但是许多日本患者会出现急性期反应(APRs)。在这项多中心、随机、开放标签、平行组研究中,研究人员评估了日本最常用的非甾体抗炎药洛索洛芬在降低唑来膦酸引起的APRs发生
唑来膦酸输液用于治疗骨质疏松症,但是许多日本患者会出现急性期反应(APRs)。在这项多中心、随机、开放标签、平行组研究中,研究人员评估了日本最常用的非甾体抗炎药洛索洛芬在降低唑来膦酸引起的APRs发生率和体温方面的疗效,并调查了该人群APRs的风险/保护因素,研究结果已在线发表于J Bone Miner Metab。

研究纳入年龄≥60岁的原发性骨质疏松症患者(n = 368),随机分配到唑来膦酸加洛索洛芬组(ZOL + LOX)或单独使用唑来膦酸组(ZOL)。所有患者在第1天接受5mg唑来膦酸输注,ZOL + LOX组患者在第1天和第2天还分别接受120mg和180mg口服洛索洛芬。在7天的观察期内,记录不良事件和体温。
结果显示,ZOL+LOX组和ZOL组的APRs发生率分别为34.4%(64/186例)和47.8%(87/182例)(P=0.0109)。两组患者体温升高(≥1℃和≥37.5℃)的比例相似(P = 0.1186)。过去双膦酸盐使用者的APRs发生率明显低于未接受治疗的患者(OR 0.444,95%置信区间0.285-0.692,P = 0.0003)。
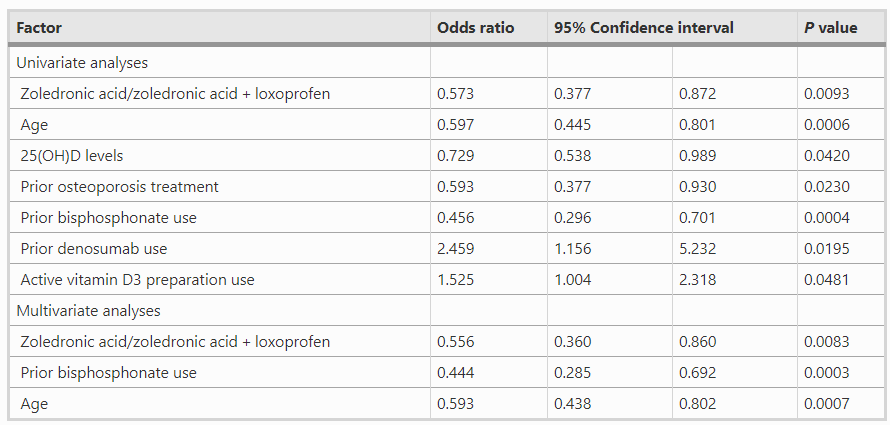
综上所述,该研究结果表明,洛索洛芬可抑制唑来膦酸诱导的APRs。已知的风险/保护因素,包括先前的骨质疏松症治疗,适用于日本患者。
原始出处:
Nobukazu Okimoto, Akinori Sakai, et al., Efficacy of non-steroidal anti-inflammatory drugs on zoledronic acid-induced acute-phase reactions: randomized, open-label, Japanese OZ study. J Bone Miner Metab. 2020 Mar;38(2):230-239. doi: 10.1007/s00774-019-01050-8.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#急性期#
51
#MET#
32
#Meta#
34
#Bone#
33
这都能发出来,受教了
73
#唑来膦酸#
31
洛索洛芬可抑制唑来膦酸诱导的急性期反应
80