Blood:EMT调控因子SNAI1通过与LSD1相互作用促进AML进展
2020-05-16 QQY MedSci原创
KDM1A/LSD1是AML的新治疗靶点。SNAI1是AML中KDM1A/LSD1靶向选择的病理调节性因子。 靶向SNAI1-LSD1复合物或其下游靶点,可能是AML的一种新颖而有效的治疗策略。
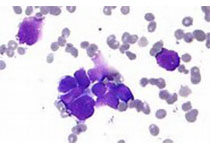
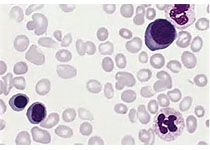
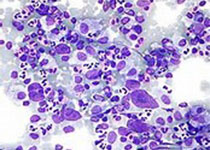
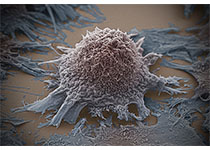
在本研究中,Carmichael等人发现,EMT的一个关键调控因子,SNAI1的过表达在人急性髓系白血病(AML)中是一种病理相关事件,可导致未成熟髓系细胞分化受损、自我更新和增殖增强。
此外,研究人员还在小鼠中证明了,Snai1在造血细胞中的异位表达可导致急性髓系白血病的发生。这种作用是通过与组蛋白去甲基酶KDM1A/LSD1的相互作用介导的。
本研究揭示了SNAI1在白血病发展中的新作用,并确定了LSD1在癌症中破坏的新机制。鉴于目前人们对LSD1抑制剂在治疗包括AML在内的多种不同恶性肿瘤的兴趣,这一点尤其重要。
原始出处:
Catherine L Carmichael,et al. The EMT modulator SNAI1 contributes to AML pathogenesis via its interaction with LSD1. Blood. May 5, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#相互作用#
0
#SNAI1#
43
#LSD1#
36
#EMT#
41
#互作#
34