Waldenström巨球蛋白血症患者同时存在 皮肤巨球蛋白病和Buschke硬肿病
2020-06-16 医学参考报皮肤病与性病学频道 医学参考报皮肤病与性病学频道
血清单克隆免疫球蛋白的存在可导致一些并发症,这些并发症是由于免疫球蛋白在体内循环和/或其沉积在如肾脏、外周神经系统和皮肤等组织所引起的。其他特殊的皮肤表现是罕见的。它们被称为具有临床意义的单克隆性丙种
血清单克隆免疫球蛋白的存在可导致一些并发症,这些并发症是由于免疫球蛋白在体内循环和/或其沉积在如肾脏、外周神经系统和皮肤等组织所引起的。其他特殊的皮肤表现是罕见的。它们被称为具有临床意义的单克隆性丙种球蛋白病(MGCS)。我们报告一位循环性IgM患者,相继出现两种不寻常的皮肤学表现:皮肤巨球蛋白病(CM)和布希克硬化性水肿(SB)。
2013年,一名56岁男子被诊断为IgM单克隆丙种球蛋白病,无特殊性临床表现,无需治疗。2016年2月,他出现丘疹,脚底覆盖一层厚厚的角化过度层(图1)。其中一个丘疹的活检显示真皮中有丰富(PAS)(+)粉红色无定形沉积物。刚果红染色(-)。免疫组化分析显示IgM重链和lambda轻链沉积。这些发现与CM的典型表现一致(图2)。2016年11月,颈部及背部出现皮肤增厚和色素沉着(图1)。组织病理学和直接免疫荧光显示结果与SB一致(图2)。患者出现贫血。骨髓活检显示细胞数量减少,淋巴细胞浆细胞间质浸润CD20+淋巴细胞,有MYD88 L265P和CXCR4 S338X突变。由于Waldenstr?m巨球蛋白血症(WM)的病程加重,我们决定每月开始用利妥昔单抗、环磷酰胺和皮质类固醇进行免疫化疗。经过治疗患者的病情好转,两处皮肤损害(图1d)和部分血液反应完全恢复。

图1.皮肤损伤
(a)有出血中心和脐窝的丘疹,可判断为皮肤巨球蛋白病。
(b)脚底有多个丘疹。
(c)颈部背部皮肤增厚,伴有Buschke硬肿病
(d)治疗巨球蛋白血症期间皮肤巨球蛋白病改善。
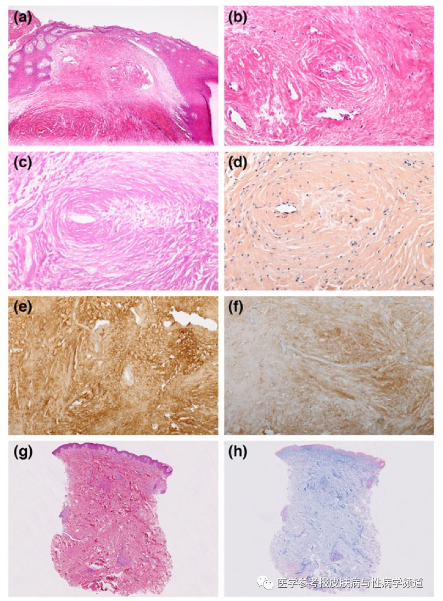
图2病变组织病理学-脚底丘疹活检(a-f),颈部活检(g,h)。
(a,b)嗜酸性无定形物质沉积于真皮、周围和血管内[苏木精/伊红染色,x50(a),x200(b)]。
(c)Pas染色(PAS x200)。
(d)刚果红染色阴性(刚果红,x200)。
(e)IgM(+)染色(x200)。
(f)lambda轻链染色(+)(x200)。
(g)皮肤硬化和轻度血管周围淋巴细胞浸润。(H/E x2.5)。
(h)阿新蓝染色(x2.5)显示轻度间质粘蛋白沉积。
IgM相关的皮肤并发症可根据其病理生理机制进行分类:或与荷瘤有关,皮肤有特异性IgM分泌的肿瘤性B细胞浸润;或与IgM理化性质有关,见于增殖性疾病或小的无痛性克隆。
无序的IgM沉积以CM为特征,由Tichenor等人首先描述。1978年被称为“巨球蛋白血症角质层”。IgM沉积呈半透明皮肤色丘疹,中心出血或呈脐窝状。
组织病理学特征显示真皮、血管周围或血管内以及血管壁内有密集的嗜酸性、PAS阳性物质。刚果红染色显示淀粉样蛋白沉积阴性。免疫组化研究或直接免疫荧光显示存在IgM。通常,这种并发症与增生性巨球蛋白血症有关。
SB是一种罕见的皮肤粘液病,发病机制不明,最早于19027、8年描述,分为三个临床组。已发现II型与单克隆性丙种球蛋白病、多发性骨髓瘤或B细胞淋巴瘤有关。患者呈现皮肤无点状硬结,大多发生在颈部、面部、胸部或上臂。组织病理学研究显示胶原纤维束增厚,间隙清晰。组织化学染色显示阿新蓝(+)、PAS(-)物质沉积与酸性粘多糖一致。直接免疫荧光对免疫球蛋白沉积呈阴性。我们在文献中发现了一个独特的案例,描述了WM和SB之间的联系。
其他已确定的机制包括有组织的IgM沉积(I型冷球蛋白血症)、IgM特异性自身免疫表现(大疱性皮肤病患者皮肤的直接靶向、II型和III型冷球蛋白血症和黄瘤病患者的10种或免疫复合物)或细胞因子分泌不当(Schnitzler综合征)。
这是第一例诊断为WM患者具有两种皮肤病事件。它强调了认识这些表现的重要性,因为它们可以先于或揭示一种进行性或复发性疾病。在没有已知的IgM单克隆丙种球蛋白病时, MGCS如存在此类表现,应在MGCS中对无痛性由懒惰克隆分泌的单克隆成分进行分析。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#球蛋白#
23
#NST#
39
#Waldenström#
33
#ALD#
25