Clin Cardiol:Lp(a)≥16 mg/dL可预测远期死亡风险,LDL-C没有这种能力
2017-05-05 卢芳 中国循环杂志
广东省人民医院周颖玲、刘勇等进行的研究显示,对于冠脉造影或接受介入治疗(PCI)患者,Lp(a)水平升高可独立预测远期死亡风险,而LDL-C水平不能预测。
广东省人民医院周颖玲、刘勇等进行的研究显示,对于冠脉造影或接受介入治疗(PCI)患者,Lp(a)水平升高可独立预测远期死亡风险,而LDL-C水平不能预测。
研究显示,不同水平Lp(a)水平患者在院内死亡率相似,但在中位随访1.95年时,Lp(a)≥16 mg/dL者死亡率明显升高,为5.8%,而<16 mg/dL者为2.5%。图1
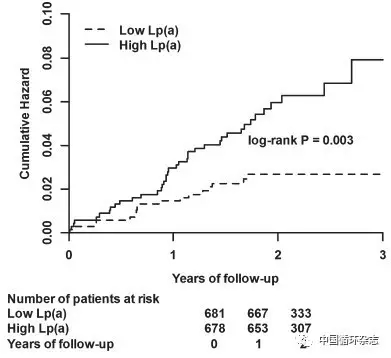
图1 不同Lp(a)水平者的远期死亡风险不同
校正相关混杂因素后,进一步分析发现,Lp(a)≥16 mg/dL可独立预测患者远期死亡风险(HR=1.96)。
研究者介绍说,在受试患者中,有94%的人在坚持服用他汀,但他汀对Lp(a)效果不大,就目前而言,新药PCSK9抑制剂以及烟酸有助于降低Lp(a)水平。
该研究共纳入1684例接受冠脉造影或PCI者,其中842人Lp(a)水平较低<16 mg/dL,另有842人Lp(a)水平较高≥16 mg/dL。
原始出处:
Feng Z, Li HL, Bei WJ, et al. Association of lipoprotein(a) with long-term mortality following coronary angiography or percutaneous coronary intervention. Clin Cardiol. 2017 Apr 26.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Cardiol#
27
#死亡风险#
30
#LDL#
27
学习了,谢谢
54