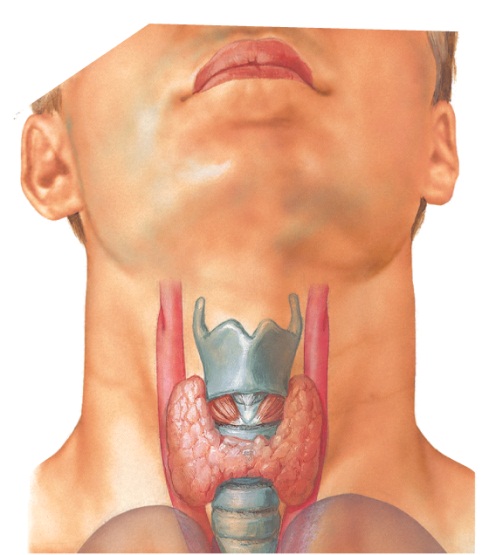
Endocr Pract:原发性甲状旁腺功能亢进症患者的维生素D研究
2016-10-05 Mechront 译 MedSci原创
研究数据显示,健康成人和原发性甲状旁腺功能亢进成年患者,其自由和生物有效性25羟维生素D水平是相似的。 不过,原发性甲状旁腺功能亢进症成年患者的血清25(OH)D水平更低。 来自罗伯特木材约翰逊医学院的Xiangbing Wang博士称:较低的25(OH)D水平可能反映不出原发性甲状旁腺功能亢进症患者的真正维生素D状态。 Wang和他的同事评估了50名原发性甲状旁腺功能亢进症成年
研究数据显示,健康成人和原发性甲状旁腺功能亢进成年患者,其自由和生物有效性25羟维生素D水平是相似的。
不过,原发性甲状旁腺功能亢进症成年患者的血清25(OH)D水平更低。
来自罗伯特木材约翰逊医学院的Xiangbing Wang博士称:较低的25(OH)D水平可能反映不出原发性甲状旁腺功能亢进症患者的真正维生素D状态。
Wang和他的同事评估了50名原发性甲状旁腺功能亢进症成年患者(平均年龄58.3岁)和50名年龄、性别和体重指数相匹配的对照组(平均年龄58岁),探究自由和生物有效性25(OH)D水平的组间差异。
总的来说,36%的原发性甲状旁腺功能亢进症患者,其25(OH)D水平低于20 ng/mL。与对照组相比,原发性甲状旁腺功能亢进症患者的总25(OH)D水平和维生素D结合蛋白水平更低(P < .01)。
两组参与者有相似的白蛋白结合25(OH)D水平;但是对照组维生素D结合蛋白25-(OH)D水平更高(P < .01)。原发性甲状旁腺功能亢进症患者的白蛋白水平低于对照组(P < .05)。
研究者发现,血清维生素D结合蛋白水平和甲状旁腺激素、钙水平之间呈负相关(P < .01);血清维生素D结合蛋白水平与25-(OH)D(P < .05)和白蛋白水平(P < .05)水平之间呈正相关。
研究者称:我们的研究结果表明,总25(OH)D水平可能不能够准确的反应原发性甲状旁腺功能亢进症患者的生物有效性25羟维生素D水平。临床医生应该意识到,原发性甲状旁腺功能亢进症患者出现低水平25-(OH)D,可能存在高钙血症恶化。未来需要进一步调查维生素D结合蛋白、25-(OH)D和原发性甲状旁腺功能亢进症病因之间的联系。
原始出处:
Total serum 25-(OH)D levels lower in primary hyperparathyroidism vs. healthy adults.Helaio.October 4, 2016
Wang X, et al. FREE AND BIOAVAILABLE 25-HYDROXYVITAMIN D LEVELS IN PATIENTS WITH PRIMARY HYPERPARATHYROIDISM.Endocr Pract. 2016;doi:10.4158/EP161434.OR.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#原发性#
30
#甲状旁腺功能亢进#
32
#甲状旁腺#
28
#原发性甲状旁腺功能亢进#
26
謝謝分享,,,
71
很不錯的文章,,
73
學習啦,,,
67
继续关注!
55
谢谢分享!
58
谢谢分享!
26