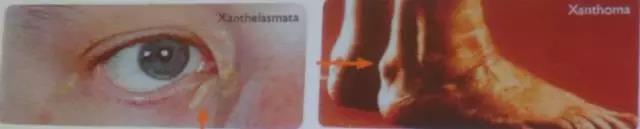
你有没有漏诊过这种病:家族性高胆固醇血症
2017-09-13 光啊 医学界心血管频道
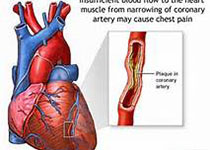
9月8-11日,由国际罕见病与孤儿药大会、罕见病发展中心、北京协和医院共同举办的“第十二届国际罕见病与孤儿药大会暨第六届中国罕见病高峰论坛”在北京隆重开幕。本文来自北京阜外心血管病医院李建军教授的演讲,针对心内科罕见病——家族性高胆固醇血症。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









学习了.
69
#家族性#
0
#漏诊#
32
#高胆固醇血症#
28
学习了.见识增长
62
学习.谢谢分享
66
学习了谢谢分享
61
谢谢分享.学习了
67
好好学习.多看看
18
学习一下
27