Clin Oncol:FOLFIRI联合贝伐珠单抗对比FOLFIRI联合阿柏西普二线治疗转移性结直肠癌的疗效
2022-03-21 yd2015 网络
研究表明,FOLFIRI联合贝伐珠单抗对比FOLFIRI联合阿柏西普二线治疗转移性结直肠癌(mCRC)疗效相当。
近期,Clinical Oncology杂志上发表了一项临床研究成果,主要是在一线奥沙利铂为基础化疗失败的转移性结直肠癌(mCRC)患者中,二线使用FOLFIRI联合贝伐珠单抗对比FOLFIRI联合阿柏西普治疗的疗效。
我们分析了2017年10月-2020年3月期间接受FOLFIRI联合贝伐单抗或阿柏西普作为二线治疗mCRC的患者的治疗结果。该分析包括67名接受FOLFIRI加阿柏西普的患者和83名接受FOLFIRI加贝伐单抗的患者。
150例患者中,男性75例(50.0%),女性75例(50.0%)。结肠右侧是原发肿瘤最常见的部位(62.6%),76例患者发现RAS基因突变(50.6%)。在二线治疗开始时,所有患者东部肿瘤合作组(ECOG)评分为0-1。FOLFIRI+阿柏西普组中位年龄为56.0岁,FOLFIRI+贝伐珠单抗组中位年龄为57.4岁。两组患者的临床特征差异无统计学意义。
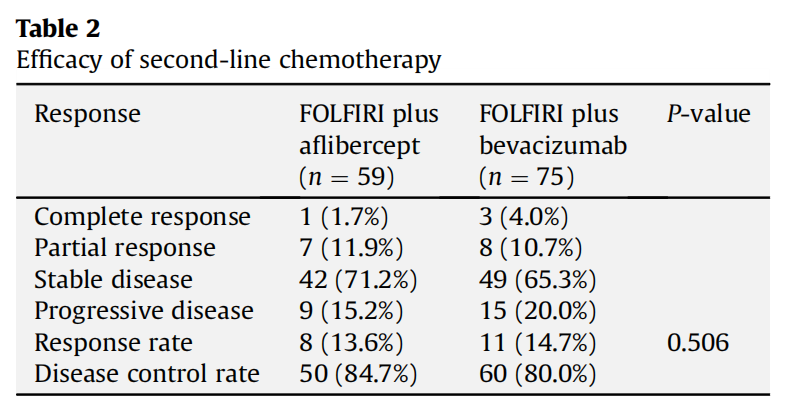
FOLFIRI+阿柏西普组的总缓解率(ORR)为13.6%(95%CI 4.85-22.34),包括1例CR,7例PR。DCR为84.8% (95%CI 75.63-93.96)。FOLFIRI+贝伐珠单抗组的总缓解率(ORR)为14.7%(95%CI 6.68-22.71)。包括3例CR,8例PR。DCR为80.0% (95%CI 70.94-89.05)。两组的ORR和DCR差异无统计学意义。
FOLFIRI+贝伐珠单抗组中位PFS为8.6个月,FOLFIRI+阿柏西普组中位PFS为8.5个月,两组中位PFS差异没有统计学差异(P=0.752)。

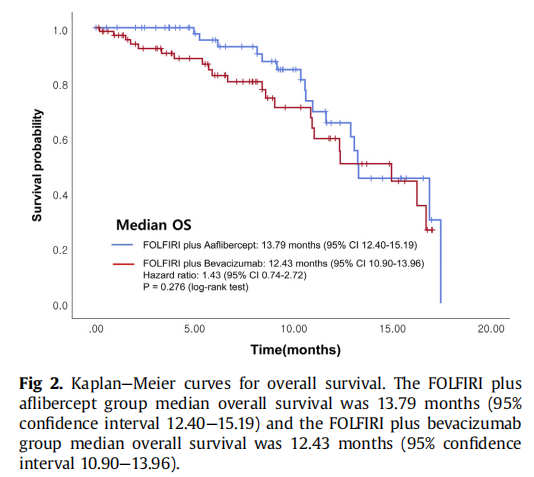
FOLFIRI+贝伐珠单抗组患者的中位OS为12.4个月,而FOLFIRI+阿柏西普组患者的中位OS为13.7个月,两组患者的OS无显著差异(P=0.276)。
在接受FOLFIRI+阿柏西普组治疗的患者中,有86.5%报告了任何级别的治疗相关不良事件,在接受FOLFIRI +贝伐珠单抗治疗的患者中,有83.1%报告了治疗相关不良事件。FOLFIRI+阿柏西普组中有11.9%的患者报告了3级或4级不良事件,FOLFIRI +贝伐珠单抗组中有2.4%的患者报告了3级或4级不良事件。最常见的不良反应是厌食症,其次是恶心、高血压、中性粒细胞减少和粘膜炎。两种方案不良事件发生率差异无统计学意义。然而,3级或3级以上的高血压在FOLFIRI+阿柏西普组组更常见。

综上,研究表明,FOLFIRI联合贝伐珠单抗对比FOLFIRI联合阿柏西普二线治疗转移性结直肠癌(mCRC)疗效相当。
原始出处:
Jo H, Lee MS, Lee YP, Kim H, Hong JY, Lee J, Park SH, Park JO, Park YS, Lim HY, Kang WK, Kim ST. A Comparison of Folinic Acid, Fluorouracil and Irinotecan (FOLFIRI) plus Bevacizumab and FOLFIRI plus Aflibercept as Second-line Treatment for Metastatic Colorectal Cancer. Clin Oncol (R Coll Radiol). 2022 Mar 2:S0936-6555(22)00095-4. doi: 10.1016/j.clon.2022.02.011. Epub ahead of print. PMID: 35248464.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#贝伐珠#
46
#Oncol#
37
#转移性#
41
#阿柏西普#
48
#结直肠#
43
#贝伐#
44
#FOLFIRI#
41
#二线治疗#
54