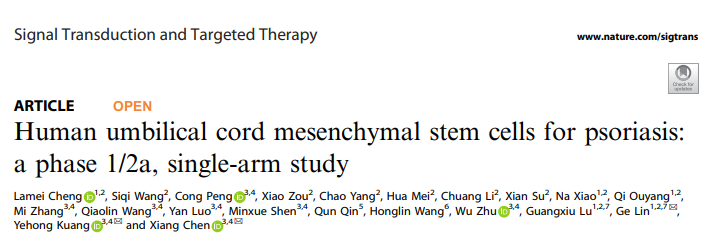
Signal Transduct Target Ther:研究揭示人脐带间充质干细胞治疗银屑病的疗效及机制
2022-08-27 MedSci原创 MedSci原创
银屑病是一种常见的、慢性免疫介导的系统性疾病,没有有效和持久的治疗方法。间充质干细胞(MSCs)的免疫调节能力使其成为临床研究中治疗自身免疫性疾病的候选者。
银屑病是一种常见的、慢性免疫介导的系统性疾病,没有有效和持久的治疗方法。间充质干细胞(MSCs)的免疫调节能力使其成为临床研究中治疗自身免疫性疾病的候选者。既往研究显示,两例通过脐带衍生间充质干细胞治疗的寻常型银屑病患者显示,这两名患者都保持了四年或五年的无复发期。近日,发表于 Signal Transduct Target Ther 的一项 1/2a 期单臂临床试验评估了人脐带间充质干细胞(UMSCs)治疗银屑病的安全性和有效性,并初步探索其可能的机制。
研究共纳入了17名银屑病患者,接受了UMSC输液。对不良事件、实验室参数、PASI和PGA进行了记录和分析。
结果,在治疗和6个月的随访中,研究人员并没有观察到明显的副作用。共有47.1%(8/17)的银屑病患者的PASI评分有至少40%的改善,根据PGA评分,17.6%(3/17)的患者没有疾病迹象或疾病极轻。男性的有效率为25%(2/8),女性为66.7%(6/9)。UMSC移植(UMSCT)后,银屑病患者外周血(PB)中Tregs和CD4+记忆T细胞的频率明显增加,而T辅助(Th)17和CD4+幼稚T细胞的频率则明显下降。所有应答者的Tregs和CD4+记忆T细胞明显增加,而Th17细胞和血清IL-17水平在UMSCT后明显下降。而且应答者的Tregs基线水平明显低于非应答者的水平。
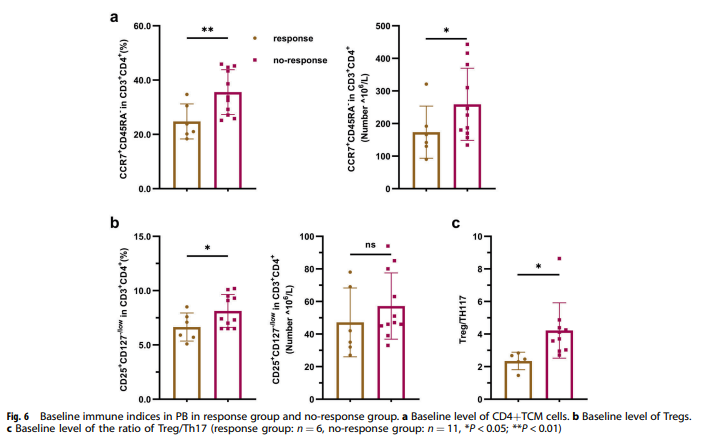
综上所述,该研究结果表明,同种异体移植对银屑病患者是安全和部分有效的,Tregs水平可作为预测同种异体移植临床疗效的有效生物标志物。
原始出处:
Lamei Cheng, et al., Human umbilical cord mesenchymal stem cells for psoriasis: a phase 1/2a, single-arm study. Signal Transduct Target Ther. 2022 Aug 5;7(1):263. doi: 10.1038/s41392-022-01059-y.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Sign#
46
#TRA#
40
#间充质干细#
45
#Signal#
56
#target#
62
#脐带#
41