Alzheimer Dementia : 磷酸化tau蛋白,比总tau蛋白和神经丝轻链更能预测痴呆
2021-12-09 Freeman MedSci原创
血浆p-tau181用于检测AD痴呆,以及使用基于血液的生物标志物进行最佳疾病检测。
美国国家老龄化研究所和阿尔茨海默氏症协会(NIA-AA)研究框架通过其潜在的病理生理过程定义了阿尔茨海默氏症(AD)。测量AD神经病理变化的体内生物标志物对于AD的早期检测和治疗至关重要。生物标志物有三种分类:脑淀粉样变(A)、神经变性(N)和tau病理(T)。
脑脊液(CSF)和正电子发射断层扫描(PET)成像是检测AD病理生理学的黄金标准,为识别淀粉样β(Aβ)和高磷酸化tau(p-tau)提供了一个进入中枢神经系统(CNS)的直接窗口。磁共振成像(MRI)是评估神经元损失(如萎缩)的常规方法,但CSF分析蛋白质,如总tau(t-tau)和神经丝光(NfL),也能深入了解神经变性的严重程度。这些方法被认为是侵入性的和/或昂贵的,因此需要具有类似准确性的可扩展生物标志物测量。开发更实用的生物标志物将允许在研究和临床环境中大规模实施。
通过超灵敏的免疫测定和质谱技术的进步,可以在血液中检测到低丰度的蛋白质,为生物标志物的开发提供了一个令人兴奋的途径。在AD和AD相关痴呆症领域,神经变性的血浆生物标志物一直备受关注,特别是NfL和t-tau,它们反映了神经元损伤和细胞死亡或变性。Sugarman等人发现,较高的血浆NfL水平可将AD痴呆症与正常认知(NC)和轻度认知障碍(MCI)的患者区分开来;此外,血浆NfL与疾病的严重程度和多个领域的神经心理测试表现恶化有关,无论是在基线还是纵向上。血浆t-tau的结果不太乐观,它只能区分AD痴呆和NC,与神经心理学功能的相关性较弱,而且不能预测纵向结果。这些结果与以前的研究是一致的,这些研究支持血浆NfL是比t-tau更准确的AD神经变性的生物标志物。
最近的探究针对免疫测定的发展来检测血液中的p-tau。高磷酸化tau是AD病理学的标志,也是AD神经变性和认知及功能下降的前兆,使其成为生物标志物研究的明确目标,以促进疾病的检测、诊断和评估治疗反应。随着p-tau免疫测定技术的新发展,血浆p-tau显示出作为AD病理的一个可行的生物标志物的潜力。虽然CSF中测量的多种tau磷酸化形式支持检测AD型tau病理,如苏氨酸217(p-tau217)和苏氨酸231(p-tau231),但苏氨酸181(p-tau181)在早期血浆生物标志物分析中已被广泛描述。 血浆中的p-tau181浓度与神经心理学测试表现恶化有关,与纵向灰质萎缩和转化为AD痴呆的几率增加相关,并将AD痴呆与其他神经退行性疾病(如。额颞叶变性)。此外,在最近的一项尸检研究中,血浆p-tau181对AD病理有很高的预测性;尽管是在死前8年采集的,但该生物标志物对死后的AD tauopathy是敏感的。
关于血浆p-tau181准确检测AD临床表现的能力的研究仍处于起步阶段。现有的研究集中在p-tau181上;血浆p-tau181与其他血浆生物标志物相比,以及与其他血浆生物标志物相结合的诊断效用仍不清楚。这是一个重要的局限性,因为相对于任何一种孤立的血浆蛋白,一组血浆生物标志物可能会有最佳的诊断准确性。本研究的目的是考察血浆p-tau181与认知诊断状态(即NC、AD导致的MCI和AD痴呆)之间的关联,单独和与血浆tau和NfL一起,以及测试血浆p-tau181与神经心理学测试表现之间的关联。
网络理论表明,像神经系统疾病这样的实体最好从一个包容性的方法来理解,各种预测因素和推论都要协同检查。网络模型代表了一个联合条件概率分布,其中节点(即变量)与边(即变量之间的有向或无向关联)相连。这些模型是理解复杂系统的数据驱动的尝试。虽然没有得到充分利用,但网络模型已被用于AD的生物标志物研究,,最近还被用于一项基于血液的生物标志物研究。
波士顿大学的Brandon Frank等人,使用Simoa平台对235名认知正常(NC)的参与者、181名因AD导致的轻度认知障碍(MCI)的参与者和153名AD痴呆患者的血浆样本进行了分析。统计学方法包括多叉回归和高斯图形模型(GGMs),以评估血浆生物标志物、神经心理学测试和人口统计学变量的网络。
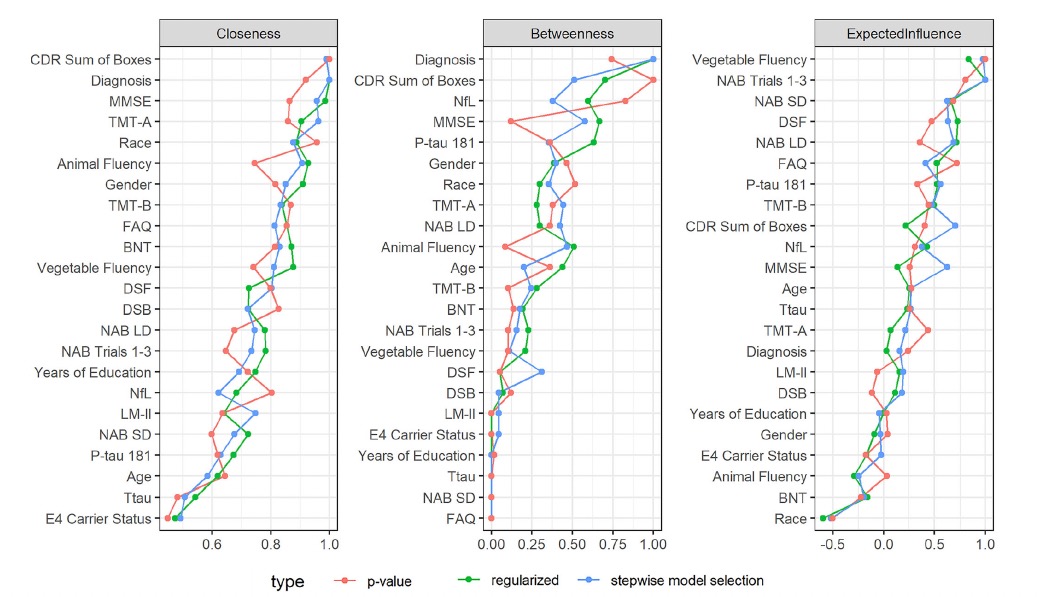 他们发现:血浆p-tau181可以区分AD痴呆和NC,但不能区分MCI,并与痴呆严重程度和更差的神经心理测试表现相关。
他们发现:血浆p-tau181可以区分AD痴呆和NC,但不能区分MCI,并与痴呆严重程度和更差的神经心理测试表现相关。
血浆NfL同样可以区分诊断组。与血浆NfL或t-tau不同,p-tau181在引导的GGM中与认知诊断有直接联系。
这个研究的重要意义在于发现了:血浆p-tau181用于检测AD痴呆,以及使用基于血液的生物标志物进行最佳疾病检测。
原文出处:
Frank B, Ally M, Brekke B, et al. Plasma p‐tau 181 shows stronger network association to Alzheimer’s disease dementia than neurofilament light and total tau. Alzheimer’s & Dementia. Published online December 2, 2021:alz.12508. doi:10.1002/alz.12508
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#神经丝轻链#
52
#dementia#
37
#神经丝#
36
#Tau#
42
老年性痴呆,未来还是希望借助神经电生理吧,也许更为有效!
27